Reaching the six-week milestone after bunion surgery represents a pivotal moment in your recovery journey. At this stage, your foot has undergone significant healing, with bone cuts beginning to fuse and soft tissues starting to regain their structural integrity. The transition from post-surgical footwear to regular shoes becomes a critical consideration, as the wrong choice can compromise months of healing progress or set back your return to normal activities.
The importance of selecting appropriate footwear at this juncture cannot be overstated. Your foot remains vulnerable to pressure, swelling, and mechanical stress, yet it requires gradual reintroduction to weight-bearing activities. The shoes you choose will directly influence how effectively your foot adapts to increased mobility while protecting the surgical site from complications. Understanding the intricate balance between support, comfort, and healing requirements forms the foundation for making informed footwear decisions during this crucial recovery phase.
Post-surgical foot anatomy and healing timeline at six weeks
Bunion osteotomy recovery phases and tissue regeneration
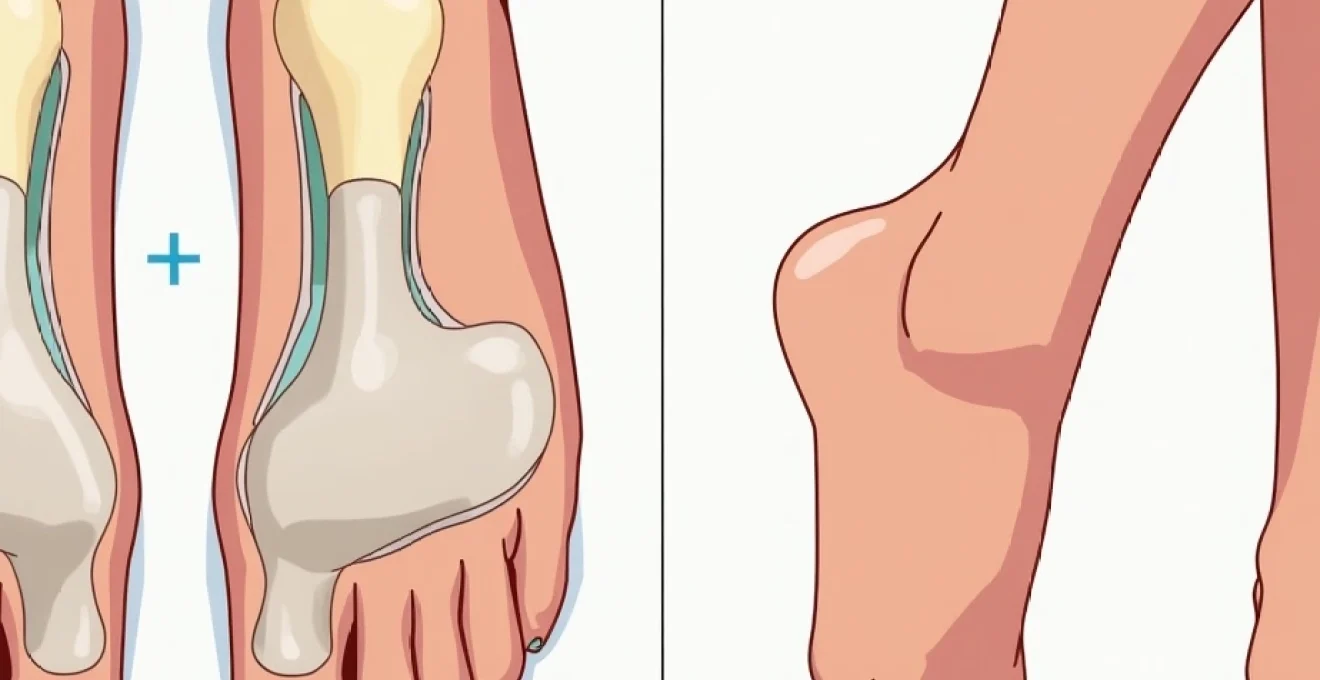
The complexity of bunion correction surgery extends far beyond simply removing the bony prominence. During the procedure, surgeons perform precise osteotomies—controlled bone cuts—to realign the first metatarsal and restore proper joint mechanics. By six weeks post-surgery, these bone cuts have entered the consolidation phase, where new bone formation actively bridges the surgical gaps. This process, known as callus formation, creates a scaffolding structure that will eventually mature into solid, healed bone over the subsequent months.
Soft tissue healing progresses simultaneously, with ligaments, tendons, and joint capsules adapting to their new anatomical positions. The plantar fascia and intrinsic foot muscles begin regaining their functional capacity, though full strength and coordination typically require several more months to develop. Understanding these biological processes helps explain why footwear selection remains critical—your foot is essentially learning to function with its corrected architecture while still healing from the surgical intervention.
Metatarsal bone fusion progress and Weight-Bearing capacity
At the six-week mark, X-rays typically reveal early signs of bone healing, though complete fusion remains months away. The surgical screws or plates used to secure the osteotomy provide mechanical stability, but the biological healing process determines your foot’s true weight-bearing capacity. Most surgeons allow patients to transition from post-surgical shoes to supportive trainers at this point, recognising that controlled mechanical stress actually promotes healthy bone remodelling.
However, the metatarsal bones remain susceptible to displacement if subjected to excessive forces. This vulnerability explains why activities involving running, jumping, or prolonged standing on hard surfaces remain prohibited. The gradual loading protocol initiated at six weeks serves a dual purpose: preventing complications while stimulating the cellular activity necessary for robust bone healing. Your choice of footwear directly influences this delicate balance between protection and progressive loading.
Soft tissue inflammation reduction and swelling management
Swelling represents one of the most persistent challenges during bunion surgery recovery, often continuing for four to six months post-operatively. At six weeks, the acute inflammatory phase has largely resolved, but residual oedema remains common, particularly after periods of activity or at the end of the day. This swelling pattern creates unique fitting challenges for footwear selection, as shoes that feel comfortable in the morning may become constrictive by evening.
The lymphatic drainage system gradually improves its efficiency as healing progresses, but mechanical factors significantly influence swelling patterns. Shoes with inadequate room for volume fluctuations can create pressure points that impede circulation and perpetuate inflammation. Conversely, footwear that accommodates swelling while providing appropriate support helps normalise tissue fluid dynamics and promotes healing. This principle underlies many of the specific design requirements for six-week recovery shoes.
Scar tissue formation around surgical incision sites
Surgical incisions continue remodelling well beyond the six-week mark, transitioning from the proliferative phase to the maturation phase of healing. During this period, collagen fibres reorganise and strengthen, but the tissue remains more sensitive to mechanical stress than normal skin. Scar tissue formation can create areas of reduced flexibility and increased sensitivity, particularly where incisions cross natural skin tension lines or joint creases.
Footwear design becomes crucial in managing these healing incisions, as pressure points or rubbing can disrupt the delicate remodelling process. Breathable materials help maintain optimal moisture levels around healing tissue, while seamless construction in critical areas prevents irritation. The psychological comfort of knowing your shoes won’t aggravate sensitive surgical sites contributes significantly to confidence in resuming normal activities during this transitional period.
Essential footwear features for bunion surgery recovery
Wide toe box construction and forefoot accommodation
The fundamental requirement for post-bunion surgery footwear centres on providing adequate space for the surgically corrected foot structure. A wide toe box serves multiple critical functions: it accommodates residual swelling, prevents pressure on healing tissues, and allows the toes to assume their new anatomical positions without constraint. The ideal toe box extends both laterally and vertically, creating a three-dimensional space that mirrors the foot’s natural contours rather than forcing adaptation to an artificial shoe shape.
Many patients underestimate the degree of width required during the six-week recovery phase. Swelling can increase foot width by up to 10-15% compared to pre-surgical measurements, and this expansion often persists for months. Additionally, the surgical correction itself may alter foot dimensions, particularly in cases involving significant angular corrections or soft tissue releases. Footwear that appeared adequate pre-surgery may become completely inappropriate during recovery, necessitating temporary sizing adjustments.
Rigid sole support systems and arch stabilisation
The importance of sole rigidity in post-bunion surgery footwear cannot be overstated. A firm, non-flexible sole serves as an external splint, limiting excessive motion at the healing osteotomy sites while distributing forces evenly across the foot. This mechanical support proves particularly crucial during the six-week period when bone healing remains incomplete and the foot’s intrinsic stabilising mechanisms have not yet fully recovered.
Arch support assumes heightened significance during bunion recovery, as the surgical correction often alters the foot’s biomechanical relationships. The first ray, comprising the big toe and first metatarsal, plays a crucial role in arch stability and propulsion during walking. While this structure heals, external arch support helps maintain proper foot mechanics and prevents compensatory problems in other areas. Built-in arch support systems prove superior to removable insoles during early recovery, as they provide consistent, reliable support that cannot shift or become displaced.
Adjustable closure mechanisms for swelling fluctuations
Traditional lacing systems often prove inadequate for managing the variable swelling patterns common during bunion surgery recovery. Adjustable closure mechanisms, including Velcro straps, BOA dials, or elastic lacing systems, allow real-time accommodation of volume changes throughout the day. This adaptability prevents the constriction that can occur with conventional shoes when swelling peaks in the afternoon or evening hours.
The positioning of closure mechanisms requires careful consideration in recovery footwear. Multiple adjustment points distributed across the forefoot and midfoot allow precise fitting control while avoiding pressure concentration over sensitive surgical sites. Some patients find that asymmetric closure systems work best, as swelling patterns often differ between the medial and lateral aspects of the foot following bunion correction.
Heel height specifications and biomechanical alignment
Heel height recommendations for six-week post-bunion surgery footwear typically range from completely flat to a maximum of 2-3cm elevation. This specification stems from biomechanical principles governing forefoot pressure distribution and first ray loading patterns. Excessive heel height shifts weight forward onto the healing surgical site, potentially disrupting bone healing and causing pain or complications.
However, completely flat shoes present their own challenges for some patients, particularly those accustomed to wearing heeled footwear pre-operatively. A modest heel elevation of 10-15mm can improve comfort and gait patterns while remaining within safe parameters for healing tissues. The key lies in selecting footwear with graduated heel-to-toe drops that promote natural walking mechanics without overloading the surgical area.
Medical-grade recovery footwear recommendations
The transition from post-surgical shoes to regular footwear at six weeks requires careful selection of intermediate recovery shoes that bridge the gap between medical devices and everyday footwear. Several categories of shoes meet the stringent requirements for this critical phase, each offering distinct advantages depending on individual needs and lifestyle factors.
Athletic trainers specifically designed for foot problems represent the gold standard for six-week recovery footwear. Brands such as New Balance, ASICS, and Brooks offer models with extra-wide toe boxes, removable insoles, and superior arch support systems. The New Balance Fresh Foam series particularly excels in providing the combination of cushioning and stability required during early recovery. These shoes feature engineered mesh uppers that accommodate swelling while maintaining structural integrity, and their Fresh Foam midsoles deliver shock absorption without compromising ground contact feedback.
Orthopedic walking shoes present another excellent option, particularly for patients who prioritise maximum comfort and accommodation over athletic performance. Companies like Orthofeet and Drew Shoes specialise in footwear designed for sensitive feet, incorporating features such as extra-depth construction , seamless interiors, and protective toe guards. These shoes often include removable insoles that can be replaced with custom orthotics as recovery progresses, providing a seamless transition to long-term foot management strategies.
For patients requiring maximum adjustability, post-surgical sandals with medical-grade construction offer unparalleled customisation. These designs typically feature multiple Velcro straps, open-toe construction for swelling accommodation, and rigid rocker-bottom soles that promote natural gait patterns while protecting healing tissues. While aesthetically less appealing than enclosed shoes, these sandals provide optimal healing conditions for patients experiencing significant swelling or sensitivity issues.
The ideal recovery shoe acts as a therapeutic device, supporting healing while gradually reintroducing normal mechanical stresses to the recovering foot structure.
When selecting recovery footwear, several key considerations guide the decision-making process. First, the shoe must accommodate the specific type of bunion surgery performed, as different procedures create varying degrees of swelling and sensitivity patterns. Minimally invasive techniques may require less accommodation than traditional open procedures, but individual responses vary significantly. Second, the patient’s activity level and occupational demands influence footwear requirements, with more active individuals needing shoes that support increased mobility while maintaining protective features.
Material selection plays a crucial role in recovery shoe performance. Synthetic materials often provide superior support and durability but may compromise breathability and comfort. Natural leather offers excellent adaptability and comfort but requires longer break-in periods that may not be appropriate during early recovery. Modern engineered fabrics represent an optimal compromise, providing the stretch and breathability of textiles with the support characteristics of traditional materials.
Transitioning from Post-Surgical shoes to regular footwear
Progressive Weight-Bearing protocol implementation
The transition from post-surgical shoes to recovery footwear follows a carefully orchestrated protocol designed to gradually increase mechanical loading while monitoring tissue response. This progression typically begins with short periods of weight-bearing in supportive shoes, initially limited to 15-20 minute intervals with rest periods between activities. The gradual increase in loading time allows tissues to adapt progressively while providing opportunities to identify and address any problematic responses.
During the initial transition phase, patients should monitor several key indicators of appropriate progression. Swelling patterns serve as reliable feedback mechanisms—excessive or prolonged swelling after activity suggests the need for reduced loading or improved footwear support. Pain levels should remain manageable and should not exceed pre-activity baselines for extended periods. Any signs of increased warmth, redness, or sensitivity around surgical sites warrant immediate consultation with the surgical team and potential modification of the progression protocol.
Gait pattern rehabilitation and walking mechanics
Bunion surgery inevitably disrupts established gait patterns, as the foot must learn to function with its corrected anatomy while accommodating healing restrictions. At six weeks, many patients exhibit compensatory walking patterns developed during the early recovery phase, including shortened stride lengths, altered toe-off mechanics, and modified weight distribution patterns. The transition to recovery footwear provides an opportunity to begin normalising these movement patterns under controlled conditions.
Proper recovery footwear facilitates gait rehabilitation by providing the stability and feedback necessary for motor learning. Rocker sole designs can help patients relearn proper heel-to-toe progression, while appropriate arch support maintains optimal foot positioning throughout the gait cycle. The transition period requires patience, as muscle memory and proprioceptive awareness need time to adapt to the foot’s new biomechanical relationships. Physical therapy interventions often prove beneficial during this phase, helping patients identify and correct problematic movement patterns before they become habitual.
Activity level progression from indoor to outdoor mobility
The expansion from indoor to outdoor mobility represents a significant milestone in bunion surgery recovery, introducing new challenges related to terrain variation, weather conditions, and increased activity demands. Indoor surfaces typically provide consistent, predictable conditions that minimise stress on healing tissues. Outdoor environments introduce variables such as uneven surfaces, slopes, and weather-related hazards that require enhanced footwear performance and improved balance responses.
Recovery footwear for outdoor use must incorporate additional safety features beyond those required for indoor activities. Enhanced traction patterns become essential for navigating wet or slippery surfaces, while increased ankle support helps manage the proprioceptive challenges associated with uneven terrain. The transition to outdoor activities should follow a graduated approach, beginning with short walks on even surfaces and progressing to more challenging environments as confidence and stability improve. Weather considerations also influence footwear selection, with waterproof options becoming necessary for continued mobility during inclement conditions.
Common footwear mistakes during Six-Week recovery period
Despite the clear guidelines for appropriate recovery footwear, several common mistakes continue to compromise healing outcomes and delay return to normal activities. Understanding these pitfalls helps patients make informed decisions and avoid setbacks during this critical recovery phase.
The most frequent error involves premature return to pre-surgical footwear, particularly narrow-toed shoes or high heels that were contributing factors to the original bunion development. The psychological desire to resume normal appearance and activities often overrides medical recommendations, leading to pain, swelling, and potential complications. Fashion considerations should remain secondary to healing requirements during the initial recovery months, as compromising healing for aesthetic reasons can result in long-term problems that far exceed temporary inconvenience.
Another common mistake involves selecting shoes based solely on comfort without considering the structural support requirements for healing tissues. While cushioned footwear feels pleasant initially, excessive softness can allow harmful motion at healing osteotomy sites and contribute to delayed union or malunion complications. The analogy of a cast illustrates this principle—just as a soft cast would provide inadequate fracture stabilisation, overly flexible shoes fail to provide the mechanical support necessary for optimal bone healing.
Size selection errors represent another significant problem area, with patients often underestimating the degree of accommodation required for post-surgical swelling. The tendency to select shoes based on pre-surgical measurements or wishful thinking about swelling resolution can result in constricted footwear that impedes circulation and perpetuates inflammation. Professional fitting services prove invaluable during this period, as experienced fitters can assess current foot dimensions and predict future changes based on healing progression.
Successful recovery requires balancing the desire for normalcy with the patience necessary for complete healing—rushing the process often extends the overall recovery timeline.
Activity level miscalculations also contribute to recovery complications, with patients either remaining overly cautious and limiting beneficial loading, or progressing too aggressively and overwhelming healing tissues. The six-week period represents a transition phase where gradual activity increases provide therapeutic benefits, but excessive demands can cause setbacks. Monitoring tissue response and adjusting activity levels accordingly requires ongoing attention and communication with healthcare providers.
Finally, many patients fail to consider the long-term implications of their six-week footwear choices. The shoes selected during this period establish patterns for future footwear decisions and can influence the ultimate success of the surgical correction. Investing in high-quality recovery footwear that supports healing while beginning the transition to long-term foot health represents a wise investment in overall treatment outcomes. The cost of appropriate recovery shoes pales in comparison to the potential expenses associated with complications or revision procedures resulting from inadequate footwear support.
Podiatrist-approved shoe fitting guidelines for Post-Bunion patients
Professional shoe fitting assumes critical importance during bunion surgery recovery, as standard fitting techniques often prove inadequate for accommodating the unique challenges of healing feet. Podiatrist-approved fitting protocols incorporate medical considerations alongside traditional comfort and fit assess
ments, creating a comprehensive evaluation framework that addresses both immediate recovery needs and long-term foot health considerations.
The timing of professional fitting proves crucial for post-bunion surgery patients, as foot dimensions continue changing throughout the healing process. Six weeks post-surgery represents an optimal assessment period, as acute swelling has typically stabilised while residual oedema patterns become predictable. However, fitting assessments should account for daily variation, with measurements ideally taken during late afternoon hours when swelling reaches peak levels. This approach ensures that selected footwear will accommodate maximum foot volume rather than creating constriction during typical daily activities.
Professional fitters experienced in post-surgical footwear recognise that traditional width classifications often prove inadequate for bunion recovery patients. The healing foot may exhibit asymmetric swelling patterns, with the surgical area requiring significantly more accommodation than unaffected regions. Additionally, the corrected bone alignment may alter foot proportions permanently, necessitating different sizing strategies than those used pre-operatively. Three-dimensional foot scanning technology can provide precise measurements that account for these complex dimensional changes, ensuring optimal fit throughout the recovery period.
Podiatrist-approved fitting protocols emphasise the importance of assessing both feet independently, as surgical correction often creates temporary or permanent asymmetries between the operated and non-operated sides. Many patients require different shoe sizes for each foot during recovery, a consideration that influences both immediate footwear selection and long-term shoe purchasing strategies. Professional fitting services can provide guidance on managing these sizing discrepancies, including recommendations for shoe exchange programs or custom modifications that accommodate bilateral differences.
The fitting process must also evaluate gait patterns and weight distribution changes that occur following bunion surgery. As patients relearn normal walking mechanics, their footwear requirements may shift, necessitating periodic reassessment throughout the recovery period. Dynamic pressure mapping can identify areas of excessive loading or pressure concentration, guiding footwear modifications or orthotic recommendations that optimise healing conditions while supporting functional recovery.
Professional fitting during bunion recovery requires understanding that the foot is not simply returning to its pre-surgical state, but rather adapting to a new, corrected anatomical configuration that may have different support and accommodation requirements.
Quality assessment criteria for recovery footwear extend beyond basic fit considerations to encompass durability, materials, and construction quality factors that influence long-term performance. The shoes selected at six weeks may need to serve recovery needs for several months, making durability a key consideration alongside immediate comfort and support requirements. Professional fitters can evaluate construction quality indicators such as sole attachment methods, upper material flexibility, and hardware reliability to ensure that selected footwear will maintain its protective and supportive properties throughout extended use.
Documentation of fitting decisions proves valuable for future reference, particularly as patients transition through different recovery phases or consider long-term footwear strategies. Professional fitting records should include dimensional measurements, specific accommodation requirements, and any custom modifications made to standard footwear. This information facilitates continuity of care and helps guide future footwear decisions as healing progresses and foot dimensions stabilise. The investment in professional fitting services during the critical six-week period often pays dividends in improved comfort, faster recovery, and reduced risk of complications that could compromise surgical outcomes.