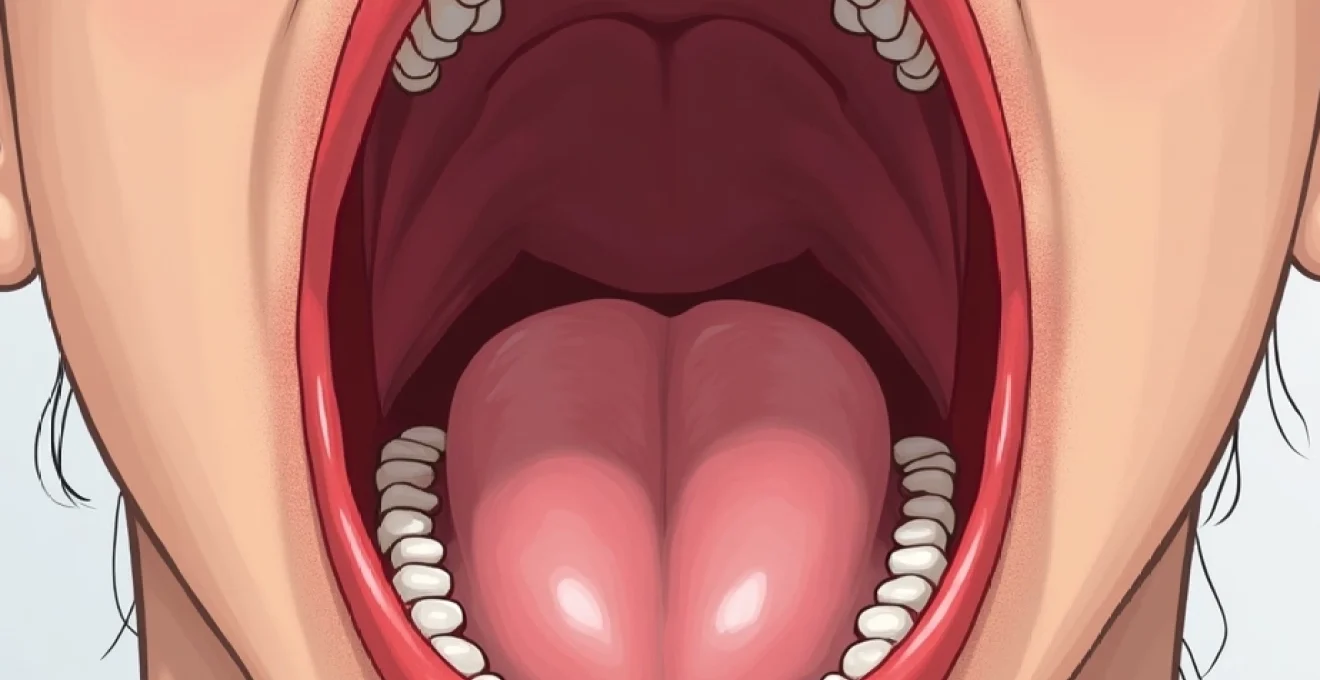
Blood blisters in the throat represent a concerning yet often misunderstood medical phenomenon that can cause significant discomfort and anxiety for patients. These haemorrhagic vesicular lesions, characterised by their dark red to purple colouration, develop when blood vessels beneath the mucosal surface rupture and blood becomes trapped within the blister cavity. Unlike their more common oral counterparts, throat-based blood blisters present unique diagnostic challenges due to their anatomical location and potential association with serious underlying conditions. Understanding the diverse aetiological factors behind these lesions is crucial for both healthcare providers and patients, as the causes range from benign traumatic incidents to complex systemic disorders requiring immediate medical intervention.
Traumatic haemorrhagic bulla formation in oropharyngeal tissues
Trauma remains the most prevalent cause of blood blister formation in the throat, accounting for approximately 70% of all cases presenting to emergency departments. The delicate mucosa lining the oropharyngeal cavity is particularly susceptible to mechanical injury due to its rich vascular supply and thin epithelial covering. When subjected to sudden pressure or shearing forces, the submucosal blood vessels can rupture whilst the overlying epithelium remains intact, creating the characteristic blood-filled cavity that defines a haemorrhagic bulla.
Traumatic blood blisters typically develop within minutes to hours of the initial injury, often accompanied by localised pain, swelling, and difficulty swallowing. The size of these lesions varies considerably, ranging from small pinpoint haemorrhages measuring just a few millimetres to large bullae exceeding two centimetres in diameter. Larger lesions pose particular risks, as they may compromise the airway or interfere with normal swallowing mechanisms.
Mechanical injury from sharp food objects and dental appliances
Sharp food items represent a significant source of oropharyngeal trauma leading to blood blister formation. Crusty bread, potato crisps, fish bones, and poorly chewed meat can create puncture wounds or abrasions in the throat tissue. The posterior pharyngeal wall and tonsillar pillars are particularly vulnerable areas where food particles may become lodged or cause scraping injuries during swallowing. Dental appliances, including ill-fitting dentures, orthodontic braces, and retainers , can create chronic irritation points that predispose to haemorrhagic bulla formation through repeated mechanical trauma.
Thermal burns from hot beverages and caustic substance exposure
Thermal injury to the throat mucosa commonly occurs through consumption of excessively hot beverages, soups, or foods heated in microwave ovens. The temperature threshold for mucosal damage begins around 60°C, with severe injuries occurring above 70°C. Chemical burns from caustic substances, including household cleaning products accidentally ingested or certain medications with high acidity levels, can also trigger haemorrhagic bulla formation as part of the inflammatory response to tissue damage.
Iatrogenic trauma during intubation and laryngoscopy procedures
Medical procedures involving instrumentation of the upper respiratory tract pose inherent risks for mucosal trauma. Endotracheal intubation, particularly in emergency settings or with difficult airways, can cause laryngeal and pharyngeal injuries leading to blood blister development. Laryngoscopy procedures, bronchoscopy, and upper endoscopy similarly carry risks of mechanical trauma to the delicate throat tissues.
Studies indicate that post-procedural haemorrhagic bullae occur in approximately 2-5% of intubation cases, with higher rates observed in patients with pre-existing coagulopathy or difficult airway anatomy.
Vigorous Coughing-Induced capillary rupture in pharyngeal mucosa
Severe coughing episodes can generate significant intrathoracic pressure changes that may lead to capillary rupture in the pharyngeal and laryngeal mucosa. This mechanism is particularly relevant in patients with chronic respiratory conditions, whooping cough, or those experiencing violent coughing fits during acute respiratory infections. The sudden pressure differentials created during forceful coughing can exceed the tensile strength of small mucosal blood vessels, resulting in localised haemorrhage and blister formation.
Infectious aetiology and Viral-Induced vesiculobullous lesions
Infectious agents represent the second most common cause of blood blisters in the throat, with viral pathogens accounting for the majority of cases. These microorganisms can directly damage mucosal tissues through cytopathic effects or indirectly cause vascular injury through inflammatory responses. The characteristic feature of infection-related blood blisters is their tendency to appear in clusters or crops, often accompanied by systemic symptoms such as fever, malaise, and regional lymphadenopathy.
Viral infections typically produce vesiculobullous lesions that may initially appear clear or fluid-filled before becoming haemorrhagic due to secondary bacterial infection or inflammatory vascular damage. The timeline for viral-induced blood blister development usually spans 3-7 days from the onset of initial symptoms, coinciding with peak viral replication and immune system activation.
Herpes simplex virus type 1 oropharyngeal manifestations
Herpes simplex virus type 1 (HSV-1) represents one of the most significant viral causes of oropharyngeal blood blisters, particularly during primary infection episodes. The virus demonstrates a strong tropism for mucosal epithelia and can cause extensive vesicular eruptions throughout the oral cavity and throat. Primary HSV-1 gingivostomatitis in adults often presents more severely than in children, with haemorrhagic bullae developing on the pharyngeal walls, soft palate, and tonsillar areas.
Epstein-barr virus mononucleosis with haemorrhagic complications
Infectious mononucleosis caused by Epstein-Barr virus (EBV) can occasionally present with haemorrhagic complications in the oropharyngeal region. The characteristic exudative pharyngitis associated with EBV infection may progress to develop blood-filled bullae, particularly in cases complicated by secondary bacterial infection or concurrent thrombocytopaenia. These lesions typically appear during the acute phase of illness and may persist for several weeks despite appropriate antiviral therapy.
Coxsackievirus Hand-Foot-and-Mouth disease pharyngeal involvement
Coxsackievirus infections, particularly those causing hand-foot-and-mouth disease, can produce characteristic vesicular lesions in the oropharyngeal cavity. While typically seen in paediatric populations, adult cases are increasingly recognised and may present with more severe manifestations. The vesicles initially appear as small, clear fluid-filled lesions but may become haemorrhagic due to trauma from swallowing or secondary bacterial contamination.
Cytomegalovirus-associated mucosal haemorrhagic bullae
Cytomegalovirus (CMV) infection can cause haemorrhagic mucosal lesions, particularly in immunocompromised patients. The virus’s ability to infect endothelial cells directly contributes to vascular fragility and bleeding tendency. CMV-associated throat lesions often present as large, painful bullae with a characteristic “owl’s eye” appearance on histological examination, reflecting the virus’s cytopathic effects on infected cells.
Systemic haematological disorders and Coagulopathy-Related causes
Haematological disorders represent a critical category of underlying conditions that predispose patients to spontaneous blood blister formation in the throat and other mucosal surfaces. These systemic conditions affect the blood’s normal clotting mechanisms, platelet function, or vascular integrity, leading to increased bleeding tendency and easy bruising. Patients with haematological disorders often present with multiple mucosal bleeding sites rather than isolated throat lesions, providing important diagnostic clues for healthcare providers.
The pathophysiology of coagulopathy-related blood blisters involves disruption of normal haemostatic mechanisms at various levels. Primary haemostatic defects affect platelet number or function, while secondary defects involve coagulation factor deficiencies or dysfunctions. Vascular disorders may also contribute through structural abnormalities of blood vessel walls, leading to increased fragility and spontaneous rupture under normal physiological pressures.
Thrombocytopaenic purpura manifesting as oropharyngeal bleeding
Thrombocytopaenic purpura, whether immune-mediated or due to decreased platelet production, commonly manifests with mucosal bleeding including blood blister formation in the throat. Idiopathic thrombocytopaenic purpura (ITP) affects approximately 3-4 individuals per 100,000 annually, with 70% of cases occurring in women.
Platelet counts below 20,000 per microlitre significantly increase the risk of spontaneous mucosal bleeding, while counts below 10,000 pose risks for life-threatening haemorrhage.
Warfarin and Anticoagulant-Induced spontaneous mucosal haemorrhage
The widespread use of anticoagulant medications has led to an increased incidence of spontaneous mucosal bleeding, including throat blood blisters. Warfarin, with its narrow therapeutic window and numerous drug interactions, poses particular risks for over-anticoagulation. Novel oral anticoagulants (NOACs), whilst having more predictable pharmacokinetics, can still cause significant bleeding complications, especially in elderly patients or those with renal impairment. The International Normalised Ratio (INR) target of 2.0-3.0 for most indications represents a balance between thrombotic and bleeding risks.
Haemophilia and von willebrand disease pharyngeal complications
Inherited bleeding disorders such as haemophilia A and B, along with von Willebrand disease, can predispose patients to mucosal bleeding episodes including throat blood blisters. Von Willebrand disease, affecting approximately 1% of the population, often goes undiagnosed until patients experience significant bleeding episodes. The disease’s variable severity means that mild cases may only become apparent during surgical procedures or dental interventions, whilst severe cases present with frequent spontaneous bleeding episodes from childhood.
Autoimmune bullous dermatoses affecting oropharyngeal mucosa
Autoimmune bullous diseases represent a complex group of conditions characterised by antibody-mediated damage to skin and mucosal surfaces. These disorders frequently involve the oropharyngeal cavity, with blood blisters forming as a result of autoimmune attack on structural proteins within the basement membrane zone or intercellular junctions. Pemphigus vulgaris and bullous pemphigoid are the most commonly encountered conditions in this category, though several other rare variants may also affect throat tissues.
The pathogenesis of autoimmune bullous diseases involves the production of pathogenic autoantibodies directed against specific structural proteins essential for maintaining tissue integrity. In pemphigus vulgaris, antibodies target desmoglein proteins responsible for cell-to-cell adhesion, leading to intraepithelial blister formation. Bullous pemphigoid involves antibodies against basement membrane proteins, resulting in subepithelial blistering with less tendency for mucosal involvement compared to pemphigus.
Diagnosis of autoimmune bullous diseases affecting the throat requires a combination of clinical presentation, histopathological examination, and direct immunofluorescence studies. The characteristic “tombstone” appearance of acantholytic cells in pemphigus vulgaris and the linear deposition of immunoglobulins along the basement membrane in bullous pemphigoid provide definitive diagnostic evidence. Treatment typically involves systemic immunosuppression with corticosteroids and adjuvant agents such as azathioprine or rituximab.
The prognosis for patients with autoimmune bullous diseases has improved significantly with modern immunosuppressive therapies, though these conditions often require long-term management. Early recognition and treatment are crucial for preventing serious complications such as secondary infection, nutritional deficiencies from painful oral lesions, and potential airway compromise from large pharyngeal bullae. Multidisciplinary care involving dermatologists, oral medicine specialists, and nutritionists often provides optimal outcomes for these complex cases.
Neoplastic and malignant processes causing haemorrhagic throat lesions
Malignant processes affecting the oropharyngeal region can present with blood blisters as an early manifestation of tumour growth and vascular invasion. Primary oropharyngeal cancers, including squamous cell carcinoma and its variants, may initially appear as innocuous blood-filled lesions before progressing to more obvious malignant characteristics. The increasing incidence of human papillomavirus (HPV)-related oropharyngeal cancers has changed the demographic profile of these diseases, with younger patients and those without traditional risk factors now presenting with throat malignancies.
The mechanism by which malignancies produce blood blisters involves several pathways. Tumour angiogenesis creates abnormal, fragile blood vessels that are prone to rupture and bleeding. Direct invasion of existing vascular structures by malignant cells can cause vessel wall weakening and subsequent haemorrhage. Additionally, tumour-associated inflammation and immune responses may contribute to vascular permeability and bleeding tendency.
Haematological malignancies, particularly leukaemias and lymphomas, can also manifest with oropharyngeal blood blisters due to their systemic effects on coagulation and platelet function. Acute leukaemia often presents with mucosal bleeding as one of the earliest symptoms, occurring before more obvious systemic manifestations become apparent. The infiltration of malignant cells into the bone marrow disrupts normal haematopoiesis, leading to thrombocytopaenia and bleeding complications.
Clinical suspicion for malignancy should be heightened in cases of blood blisters that fail to heal within 2-3 weeks, recur frequently in the same location, or are associated with other concerning symptoms such as unexplained weight loss, persistent hoarseness, or palpable lymphadenopathy.
Early detection of oropharyngeal malignancies significantly improves treatment outcomes, with five-year survival rates exceeding 80% for early-stage HPV-positive tumours compared to less than 40% for advanced-stage disease.
The diagnostic workup for suspected malignant causes of throat blood blisters should include comprehensive head and neck examination, imaging studies such as CT or MRI, and tissue sampling for histopathological analysis. The advent of minimally invasive biopsy techniques and advanced molecular diagnostic methods has improved the accuracy and speed of cancer diagnosis, enabling earlier initiation of appropriate treatment interventions.