The integration of diagnostic colonoscopy with therapeutic haemorrhoid treatment represents a significant advancement in colorectal surgery, offering patients the convenience of addressing multiple conditions during a single procedure. Recent clinical evidence demonstrates that combining colonoscopy with various haemorrhoid treatments can be both safe and effective, with studies reporting success rates exceeding 90% for symptom resolution. This approach not only optimises patient care by reducing the number of separate procedures but also maximises the efficient use of healthcare resources and minimises patient discomfort.
Modern colorectal practice increasingly recognises the value of concurrent procedures, particularly when patients present with symptomatic haemorrhoids alongside indications for colonoscopic examination. The anatomical proximity of these conditions within the same operative field makes simultaneous treatment a logical consideration, though careful patient selection and technical expertise remain paramount to achieving optimal outcomes.
Understanding concurrent colonoscopy and haemorrhoidectomy procedures
The feasibility of performing colonoscopy alongside haemorrhoidectomy depends largely on the specific surgical technique employed and the complexity of the haemorrhoidal disease. Contemporary practice has evolved to accommodate various combinations of procedures, each requiring distinct considerations regarding patient safety, operative duration, and post-operative recovery. The decision to proceed with concurrent treatment must balance the benefits of single-session intervention against the potential for increased complications.
Combined procedures typically involve standard colonoscopic examination followed immediately by haemorrhoid treatment using the same anaesthetic episode. This approach eliminates the need for separate bowel preparation regimens and reduces overall patient inconvenience. However, the extended operative time and increased physiological stress must be carefully evaluated against individual patient factors.
Anatomical considerations for combined colorectal surgery
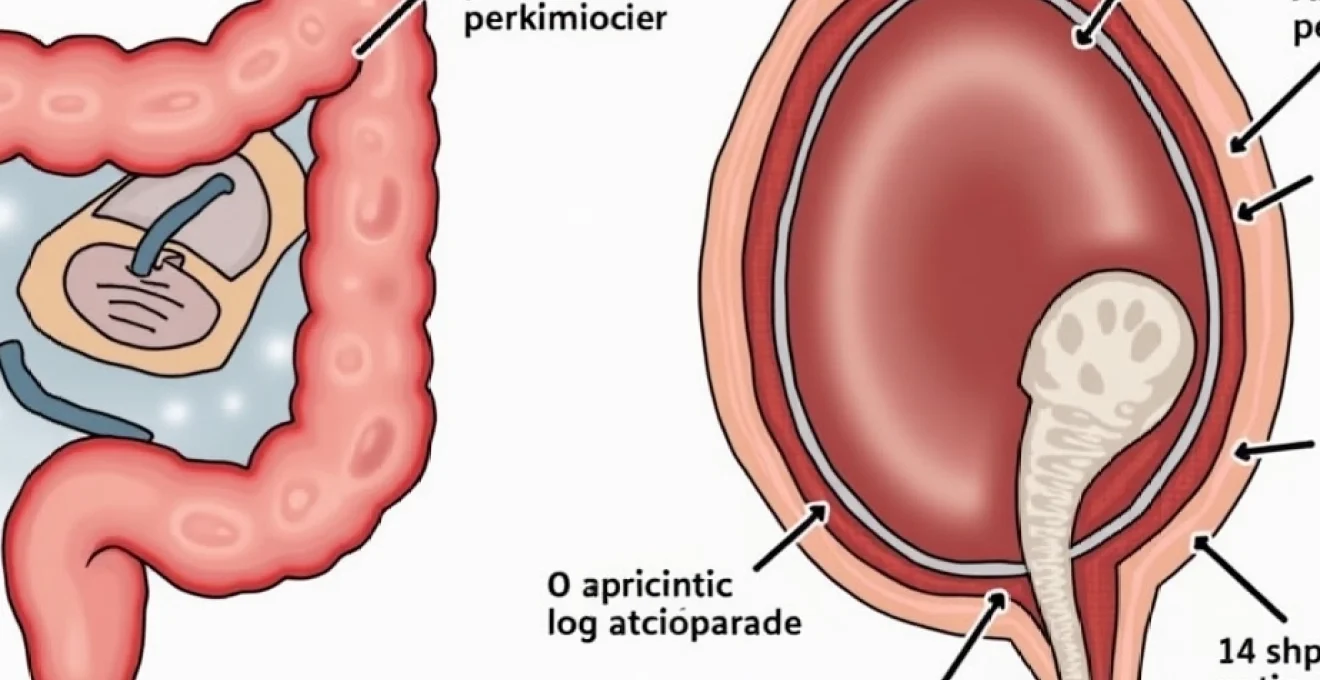
The anatomical relationship between the colon and anorectum presents unique opportunities for concurrent surgical intervention. The colonoscope’s passage through the anal canal and rectum provides an ideal opportunity to assess haemorrhoidal pathology before proceeding with therapeutic intervention. This sequential approach allows surgeons to modify their treatment strategy based on colonoscopic findings, potentially identifying additional pathology that might influence surgical planning.
Positioning considerations become particularly important during combined procedures. The standard left lateral position used for colonoscopy may need modification to accommodate subsequent haemorrhoid treatment, requiring careful coordination between the endoscopic and surgical phases of the procedure. The transition between diagnostic and therapeutic phases must be seamless to maintain optimal patient safety and procedural efficiency.
Milligan-morgan technique compatibility with endoscopic assessment
The traditional open haemorrhoidectomy technique described by Milligan and Morgan can be successfully integrated with colonoscopic examination, though this combination requires careful timing and positioning considerations. Following colonoscopic assessment, patients can be repositioned into the prone jackknife or lithotomy position for haemorrhoid excision. The open technique allows for complete visualisation of the operative field whilst maintaining the benefits of concurrent diagnosis.
Wound healing considerations become particularly important when combining these procedures, as the extended operative time and increased tissue manipulation may influence recovery patterns. Surgeons must carefully balance the thoroughness of haemorrhoidal excision against the overall physiological burden of the combined procedure, particularly in elderly or high-risk patients.
Ferguson closed haemorrhoidectomy during colonoscopic examination
The Ferguson technique offers distinct advantages when performed in conjunction with colonoscopy, as the closed wound approach may reduce post-operative complications and accelerate healing. This method involves complete excision of haemorrhoidal tissue with primary wound closure, potentially reducing the risk of secondary haemorrhage that might complicate post-colonoscopy recovery.
Technical considerations for the Ferguson technique during combined procedures include ensuring adequate haemostasis before wound closure and carefully managing the transition from endoscopic to surgical positioning. The closed nature of this technique may be particularly beneficial for patients undergoing concurrent procedures, as it potentially reduces the overall recovery burden.
Stapled haemorrhoidopexy (PPH) integration with diagnostic colonoscopy
Procedure for Prolapse and Haemorrhoids (PPH) represents perhaps the most suitable haemorrhoidal treatment for combination with colonoscopy due to its minimally invasive nature and reduced operative trauma. The circular stapling technique can be performed with minimal position changes following colonoscopic examination, maintaining procedural efficiency whilst delivering effective symptom relief.
The stapled approach offers particular advantages in terms of post-operative pain management, which becomes increasingly important when considering the combined physiological stress of dual procedures. Recovery times are typically shorter with PPH, making this technique an attractive option for patients seeking the convenience of concurrent treatment without prolonged convalescence.
Pre-operative patient assessment for combined procedures
Comprehensive pre-operative evaluation becomes critically important when considering concurrent colonoscopy and haemorrhoidectomy, as the combined physiological stress requires careful risk stratification. Patient selection must consider not only the individual pathologies requiring treatment but also the cumulative impact of extended anaesthetic exposure and increased operative trauma. Factors such as cardiovascular fitness, respiratory function, and overall physiological reserve significantly influence the appropriateness of combined intervention.
The assessment process must thoroughly evaluate both the colonoscopic indication and the severity of haemorrhoidal disease to determine whether concurrent treatment offers genuine benefit over staged procedures. Patient expectations regarding recovery time and potential complications must be carefully managed, as combined procedures may result in more complex post-operative courses compared to isolated interventions.
ASA physical status classification for dual colorectal interventions
American Society of Anesthesiologists (ASA) classification becomes particularly relevant when assessing patients for combined procedures, as higher ASA grades may preclude concurrent intervention due to increased physiological risk. ASA I and II patients generally tolerate combined procedures well, whilst ASA III patients require individualised assessment considering specific comorbidities and their potential impact on recovery.
Cardiovascular assessment assumes particular importance given the extended operative duration and potential for significant fluid shifts during combined procedures. Patients with limited cardiac reserve may benefit from staged interventions to minimise physiological stress and optimise recovery outcomes.
Bowel preparation protocols: moviprep vs citrafleet considerations
Bowel preparation regimens require modification when planning combined procedures, as the quality of colonic cleansing directly impacts both diagnostic accuracy and surgical field visualisation. Standard preparations such as Moviprep or Citrafleet remain effective for concurrent procedures, though patients must be counselled regarding the importance of complete preparation compliance given the dual therapeutic objectives.
The timing of bowel preparation becomes crucial when coordinating combined procedures, as inadequate preparation may necessitate procedure postponement with significant implications for surgical scheduling. Patient education regarding preparation protocols must emphasise the critical importance of compliance for both diagnostic and therapeutic success.
Anticoagulation management in combined Endoscopic-Surgical procedures
Anticoagulation management presents complex considerations for combined procedures, requiring careful balance between thrombotic and haemorrhagic risks. The increased bleeding risk associated with haemorrhoidal surgery must be weighed against the patient’s underlying indication for anticoagulation, often requiring multidisciplinary consultation with cardiology or haematology specialists.
Bridging protocols may need modification for combined procedures, as the extended operative time and increased bleeding risk may require longer periods of anticoagulation cessation. Individual risk assessment must consider both the underlying cardiovascular pathology and the specific surgical techniques planned for haemorrhoidal treatment.
Anaesthetic risk stratification for extended operative duration
Extended anaesthetic exposure inherent in combined procedures requires specific risk assessment, particularly regarding respiratory and cardiovascular complications. The cumulative physiological stress of prolonged anaesthesia must be balanced against the benefits of single-session treatment, with particular attention to elderly patients or those with significant comorbidities.
Anaesthetic planning must accommodate position changes between colonoscopy and haemorrhoid surgery whilst maintaining patient safety and procedural efficiency. The transition between diagnostic and therapeutic phases requires careful coordination between surgical and anaesthetic teams to ensure optimal patient outcomes.
Surgical technique modifications for simultaneous procedures
Performing colonoscopy and haemorrhoidectomy concurrently requires specific technical modifications to optimise both diagnostic accuracy and surgical outcomes. The procedural sequence typically begins with standard colonoscopic examination, allowing complete assessment of the colon whilst simultaneously evaluating the extent and severity of haemorrhoidal disease. This initial assessment phase enables surgeons to modify their therapeutic approach based on colonoscopic findings, potentially identifying additional pathology that might influence surgical planning.
Technical coordination becomes paramount during the transition from diagnostic to therapeutic intervention. The colonoscopic phase must be completed with particular attention to haemostasis if biopsies are taken, as subsequent haemorrhoidal surgery may be complicated by ongoing bleeding from proximal sites. Procedural timing requires careful orchestration to maintain optimal patient positioning and anaesthetic depth throughout both phases of treatment.
The surgical technique for haemorrhoidal treatment may require modification when performed in conjunction with colonoscopy. Standard approaches must accommodate the potential for increased bleeding risk following endoscopic intervention, particularly if polypectomy or extensive biopsy sampling has been performed. Haemostatic techniques become increasingly important, with many surgeons favouring electrocautery or harmonic scalpel technology to ensure optimal tissue sealing.
Equipment requirements for combined procedures necessitate careful pre-operative planning to ensure all necessary instruments are available without delay. The operating theatre setup must accommodate both endoscopic and surgical requirements, often requiring additional personnel to manage the transition between procedural phases efficiently. This coordination is essential to minimise overall operative duration and reduce associated complications.
Recent studies demonstrate that experienced colorectal surgeons can successfully combine these procedures with minimal increase in complication rates compared to isolated interventions, provided appropriate patient selection criteria are maintained.
Post-operative complications and management protocols
The post-operative care following combined colonoscopy and haemorrhoidectomy requires enhanced monitoring protocols due to the increased complexity and potential for complications arising from either component of the procedure. Recovery management must address the cumulative physiological stress of dual interventions whilst providing targeted treatment for specific complications that may arise from each procedural component.
Enhanced monitoring protocols typically extend beyond standard post-operative observations to include specific assessment for complications related to both colonoscopic and surgical interventions. The increased operative duration and complexity necessitate more frequent vital sign monitoring and careful assessment of fluid balance, particularly in elderly patients or those with significant comorbidities.
Haemorrhage risk assessment following combined intervention
Bleeding complications represent the most significant concern following combined procedures, as haemorrhage may arise from colonoscopic biopsy sites, polypectomy defects, or haemorrhoidal surgical sites. The cumulative bleeding risk requires careful assessment and management, with particular attention to anticoagulation timing and haemostatic adequacy at all intervention sites.
Early recognition of post-operative bleeding becomes critical, as the multiple potential bleeding sources may complicate diagnostic assessment. Patients require careful education regarding warning signs of significant haemorrhage and clear instructions for seeking immediate medical attention if concerning symptoms develop.
Anal stenosis prevention in concurrent procedure patients
The risk of anal stenosis following haemorrhoidectomy may be increased when performed in conjunction with colonoscopy due to enhanced tissue trauma and prolonged operative duration. Prevention strategies must focus on maintaining adequate anal canal diameter whilst achieving complete haemorrhoidal excision, often requiring careful balance between surgical thoroughness and functional preservation.
Post-operative anal dilatation protocols may require modification for patients undergoing combined procedures, with particular attention to patient comfort and compliance. The cumulative tissue trauma from dual interventions may necessitate more gradual progression of dilatation exercises to prevent complications whilst maintaining functional outcomes.
Infection control measures for extended operative time
Extended operative duration inherent in combined procedures increases infection risk, requiring enhanced perioperative antibiotic protocols and meticulous attention to sterile technique throughout both procedural phases. The transition from endoscopic to surgical intervention must maintain strict infection control standards to prevent contamination of surgical sites.
Post-operative wound care becomes particularly important following combined procedures, as the increased tissue trauma and extended operative time may compromise normal healing responses. Patients require detailed education regarding wound care protocols and recognition of early infection signs to ensure prompt treatment if complications arise.
Pain management protocols for dual procedure recovery
Pain management following combined procedures requires multimodal approaches addressing the cumulative discomfort from both colonoscopic and surgical interventions. Standard haemorrhoidal pain management protocols may require enhancement to accommodate additional discomfort from endoscopic procedures, particularly if extensive biopsy sampling or polypectomy has been performed.
The analgesic regimen must balance effective pain control against the potential for opioid-related complications, particularly constipation which may significantly impact recovery from haemorrhoidal surgery. Alternative pain management strategies, including regional anaesthetic techniques and non-pharmacological approaches, assume increased importance in the management of combined procedure patients.
Clinical outcomes and recovery timelines
Clinical outcomes following combined colonoscopy and haemorrhoidectomy demonstrate favourable results when appropriate patient selection and surgical technique are employed. Large-scale studies involving over 500 consecutive patients show success rates exceeding 93% for complete symptom resolution, with only 6.6% requiring repeat intervention and 2.2% needing completion surgical haemorrhoidectomy for persistent symptoms. These outcomes compare favourably with isolated haemorrhoidal treatments whilst providing the additional benefit of concurrent colonoscopic assessment.
Recovery timelines for combined procedures typically extend beyond those expected for isolated interventions, with most patients requiring 2-4 weeks for complete recovery compared to 1-2 weeks for simple haemorrhoidal treatments. The extended recovery period reflects the cumulative physiological stress of dual procedures and the increased tissue trauma associated with prolonged operative intervention. However, the overall time away from normal activities remains significantly less than would be required for staged procedures.
Functional outcomes following combined procedures generally match those achieved with isolated treatments, provided appropriate surgical technique and post-operative care protocols are maintained. Continence function typically returns to baseline within 4-6 weeks, with most patients reporting satisfactory symptom control and minimal functional impairment. Long-term follow-up data suggests durable results with low recurrence rates when adequate excision is achieved during the initial procedure.
Patient satisfaction scores consistently demonstrate high levels of approval for combined procedures, with most patients appreciating the convenience of single-session treatment despite slightly extended recovery periods. The elimination of duplicate bowel preparation regimens and separate anaesthetic exposures contributes significantly to overall patient satisfaction and willingness to recommend the approach to others with similar conditions.
Quality of life measures show significant improvement following combined procedures, with patients reporting enhanced confidence in their bowel function and reduced anxiety regarding potential complications from staged interventions.
Comparative cost analysis demonstrates economic advantages for combined procedures when considering both direct healthcare costs and indirect costs related to time away from work and multiple hospital visits. The resource efficiency achieved through concurrent treatment typically results in overall cost savings of 20-30% compared to staged interventions, making this approach attractive from both patient and healthcare system perspectives.
Contraindications and alternative treatment pathways
Absolute contraindications to combined colonoscopy and haemorrhoidectomy include severe cardiovascular compromise, significant respiratory disease limiting anaesthetic tolerance, and active inflammatory bowel disease affecting the rectum or anal canal. Patients with ASA IV classification generally require individual assessment with multidisciplinary consultation to determine procedural appropriateness and optimise perioperative management strategies.
Relative contraindications encompass conditions that increase procedural risk but may not preclude combined treatment with appropriate modifications. These include mild to moderate cardiac disease, well-controlled diabetes mellitus, and stable anticoagulation requirements that can be safely managed perioperatively. Inflammatory conditions affecting the anal canal may require staged treatment to optimise healing conditions and minimise complication risks.
Alternative treatment pathways for patients unsuitable for combined procedures include staged interventions with optimised timing to minimise overall treatment burden. Colonoscopy performed initially allows assessment of colonic pathology and planning of subsequent haemorrhoidal treatment based on findings and patient recovery. This approach may be particularly appropriate for high-risk patients or those with complex medical comorbidities requiring specialised perioperative management.
Non-surgical alternatives for haemorrhoidal treatment may be considered when combined procedures are contraindicated, including rubber band ligation, sclerotherapy, or infrared coagulation performed as office-based procedures. These minimally invasive treatments can often be combined with flexible sigmoidoscopy rather than full colonoscopy, reducing physiological stress whilst maintaining diagnostic capability for distal colonic assessment.
The decision-making process for treatment pathway selection must involve comprehensive discussion of risks, benefits, and alternatives with patients and their families. Individual patient
preferences and clinical circumstances must guide individualised treatment planning to ensure optimal outcomes and patient satisfaction.
Modern colorectal practice increasingly emphasises shared decision-making processes that incorporate patient values, preferences, and individual risk tolerance alongside clinical indicators. This collaborative approach ensures that treatment decisions align with patient expectations whilst maintaining appropriate clinical standards and safety protocols. The complexity of combined procedures necessitates thorough discussion of all available alternatives to enable fully informed consent.
Staging strategies may involve initial colonoscopic assessment followed by interval haemorrhoidal treatment once colonic pathology has been evaluated and managed appropriately. This approach allows optimisation of medical comorbidities between procedures whilst ensuring comprehensive colorectal evaluation. Sequential treatment may be particularly beneficial for patients with newly diagnosed colonic pathology requiring additional intervention or those with complex medical histories requiring specialised perioperative management.
Emergency presentation with acute haemorrhoidal complications represents an absolute contraindication to elective combined procedures, requiring immediate management of the acute condition before consideration of definitive treatment. Thrombosed external haemorrhoids, acute haemorrhoidal bleeding, or prolapsed irreducible haemorrhoids necessitate urgent intervention that precludes concurrent colonoscopic examination until the acute episode has resolved.
Age-related considerations become increasingly important when evaluating patients for combined procedures, as physiological reserve diminishes with advancing age and comorbidity accumulation. Patients over 75 years require particularly careful assessment of cardiovascular and respiratory function, with many centres adopting modified protocols or staging strategies for this population. However, chronological age alone should not preclude combined treatment if physiological assessment demonstrates adequate reserve for the proposed intervention.
The key to successful combined colorectal procedures lies in meticulous patient selection, careful surgical planning, and comprehensive post-operative care protocols that address the unique challenges of dual interventions.
Future developments in minimally invasive techniques may expand the scope of patients suitable for combined procedures, with emerging technologies offering reduced physiological stress and enhanced recovery profiles. Advances in anaesthetic techniques and pain management protocols continue to improve outcomes for complex colorectal procedures, potentially broadening the patient population that can safely undergo concurrent interventions.
The evolution of combined colonoscopy and haemorrhoidectomy represents a significant advancement in colorectal surgery, offering patients efficient, comprehensive treatment whilst maintaining safety standards and clinical effectiveness. When performed by experienced surgeons with appropriate patient selection, these procedures deliver excellent outcomes with high patient satisfaction and resource efficiency. The continued refinement of surgical techniques and perioperative care protocols ensures that this approach will remain a valuable option for suitable patients requiring both diagnostic colonoscopy and therapeutic haemorrhoidal intervention.