End-stage liver disease represents the terminal phase of chronic hepatic conditions, characterising a critical juncture where irreversible scarring and dysfunction have progressed beyond the liver’s capacity for regeneration. This advanced pathological state affects approximately 5.5 million individuals across the United States alone, with mortality rates continuing to rise globally. Understanding the complex interplay between disease progression, complications, and survival outcomes becomes paramount for patients, families, and healthcare professionals navigating this challenging medical landscape. The prognosis for end-stage liver disease varies considerably based on underlying aetiology, patient demographics, and the presence of life-threatening complications, making accurate prognostication both essential and inherently complex.
Understanding End-Stage liver disease classifications and MELD score implications
Medical professionals rely on sophisticated scoring systems to evaluate disease severity and predict survival outcomes in patients with advanced hepatic dysfunction. These classification frameworks provide standardised approaches to assess prognosis whilst informing critical treatment decisions, including liver transplantation candidacy. The evolution of predictive models has revolutionised how clinicians approach end-stage liver disease management, offering data-driven insights into patient outcomes.
Child-pugh class C decompensated cirrhosis survival rates
The Child-Turcotte-Pugh classification system remains a cornerstone in evaluating cirrhotic patients, with Class C representing the most severe manifestation of hepatic decompensation. Patients classified as Child-Pugh Class C demonstrate survival rates of approximately 59.1% at three months, declining precipitously to 45% at one year and further diminishing to 38% at two years. These stark statistics reflect the profound impact of multiple organ system dysfunction characteristic of advanced cirrhosis.
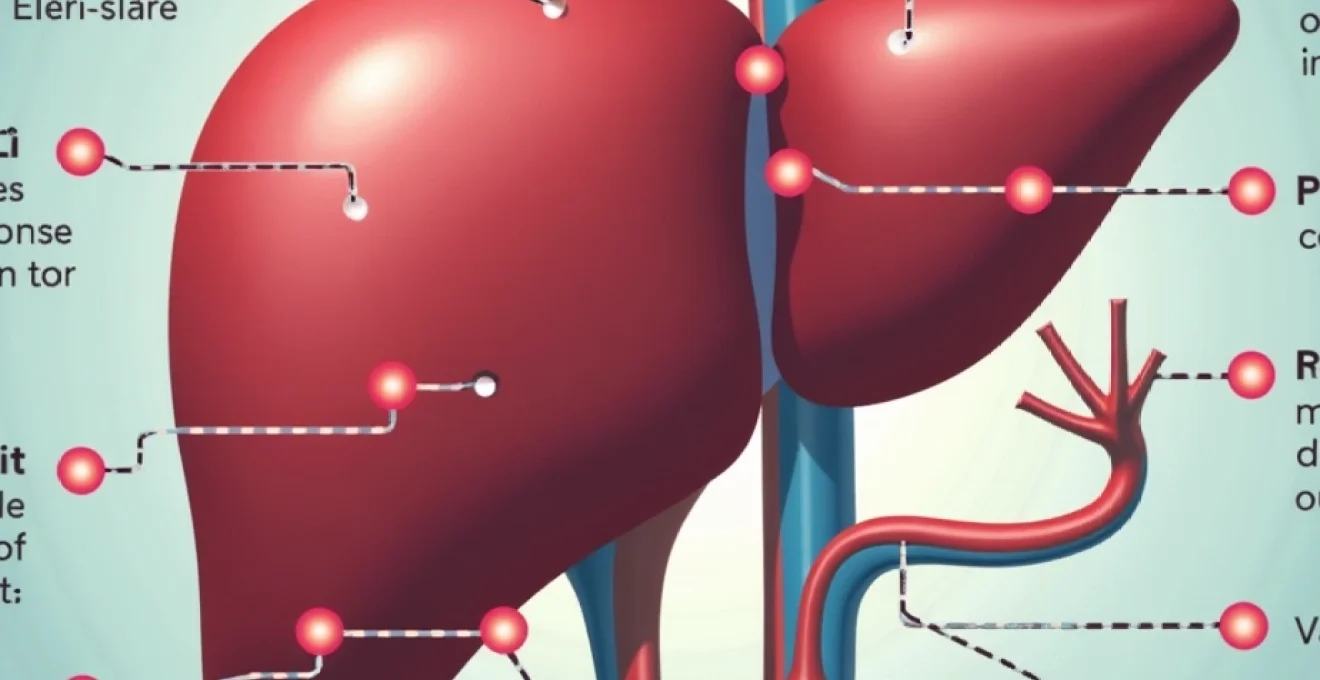
Child-Pugh Class C patients typically present with refractory ascites , severe hepatic encephalopathy, and coagulopathy that responds poorly to conventional therapeutic interventions. The scoring system evaluates five key parameters: serum bilirubin levels, serum albumin concentration, prothrombin time or international normalised ratio, presence and severity of ascites, and degree of hepatic encephalopathy. Patients accumulating 10 to 15 points across these domains qualify for Class C designation, indicating imminent risk of mortality without urgent intervention.
Model for End-Stage liver disease (MELD) score prognostic accuracy
The MELD scoring system provides more precise mortality risk stratification than traditional classification methods, incorporating objective laboratory values to generate numerical scores correlating with three-month survival probability. Contemporary MELD calculations integrate serum bilirubin, creatinine, sodium, and international normalised ratio measurements, with scores ranging from 6 to above 40. Higher MELD scores directly correlate with increased mortality risk, making this system invaluable for transplant allocation and prognostic counselling.
Recent data demonstrates that patients with MELD scores exceeding 40 face a staggering 71.3% mortality risk, whilst those scoring between 30-39 experience a 52.6% risk of death. Even moderate MELD elevations carry significant prognostic implications, with scores of 20-29 associated with 19.6% mortality rates. This granular risk stratification enables clinicians to provide more accurate survival estimates whilst prioritising high-risk patients for urgent transplant consideration.
Acute-on-chronic liver failure (ACLF) mortality predictors
Acute-on-chronic liver failure represents a distinct clinical syndrome characterised by rapid hepatic decompensation superimposed upon pre-existing chronic liver disease. This condition carries particularly ominous prognostic implications, with mortality rates reaching 50-90% depending on the number of organ failures present. The pathophysiology involves systemic inflammation, immune dysfunction, and multi-organ failure occurring within weeks of acute decompensation events.
ACLF mortality prediction relies heavily on organ failure scoring systems, with patients developing three or more organ failures facing mortality rates exceeding 80% at 28 days. The kidney represents the most commonly affected extra-hepatic organ, with renal dysfunction significantly amplifying mortality risk. Early recognition and aggressive supportive care may improve outcomes, though the window for intervention remains narrow in severely affected patients.
Hepatorenal syndrome type 1 clinical outcomes
Hepatorenal syndrome Type 1 constitutes one of the most feared complications of advanced liver disease, characterised by rapid-onset kidney failure occurring in the absence of intrinsic renal pathology. This condition develops in approximately 10% of hospitalised cirrhotic patients, carrying a median survival of just 2-4 weeks without intervention. The pathophysiology involves severe vasoconstriction of renal blood vessels coupled with splanchnic vasodilation, creating a functional kidney failure that may be reversible with appropriate treatment.
Treatment options for hepatorenal syndrome remain limited, with terlipressin and albumin representing first-line therapeutic interventions. However, response rates vary considerably, with only 30-50% of patients achieving meaningful improvement in renal function. The presence of hepatorenal syndrome Type 1 significantly elevates transplant priority, as survival without liver transplantation approaches zero in most cases. Early recognition and prompt intervention remain critical factors influencing patient outcomes in this devastating complication.
Hepatorenal syndrome type 1 clinical outcomes
Contemporary management approaches for hepatorenal syndrome have evolved to include combination therapies utilising vasoconstrictor agents alongside albumin replacement. Recent studies suggest that early intervention with terlipressin may improve response rates, particularly when initiated before serum creatinine levels exceed 2.5 mg/dL. The integration of continuous renal replacement therapy serves as a bridging strategy for transplant candidates, though outcomes remain guarded without definitive hepatic replacement.
Disease-specific survival patterns in advanced hepatic conditions
The underlying aetiology of end-stage liver disease profoundly influences survival patterns, progression rates, and response to therapeutic interventions. Different hepatic conditions demonstrate unique natural histories, with some diseases progressing more rapidly to terminal stages whilst others maintain compensated states for extended periods. Understanding these disease-specific trajectories enables more precise prognostic counselling and tailored treatment strategies.
Alcoholic liver disease End-Stage progression timelines
Alcoholic liver disease represents one of the most common causes of hepatic cirrhosis globally, with progression rates varying significantly based on continued alcohol consumption, genetic factors, and concurrent medical conditions. Patients who achieve complete abstinence from alcohol may experience stabilisation or even modest improvement in hepatic function, whilst continued drinking accelerates progression to end-stage disease. The presence of alcoholic hepatitis superimposed upon established cirrhosis carries particularly grave prognostic implications, with short-term mortality rates approaching 40-50%.
The trajectory from compensated alcoholic cirrhosis to decompensation typically occurs over 2-5 years, though individual variation remains substantial. Factors influencing progression include patient age, nutritional status, presence of viral co-infections, and adherence to alcohol cessation. Complete abstinence from alcohol remains the most critical intervention for improving survival outcomes, with some patients experiencing remarkable hepatic recovery even in advanced disease stages.
Non-alcoholic steatohepatitis (NASH) cirrhosis mortality data
Non-alcoholic steatohepatitis has emerged as a leading cause of end-stage liver disease, particularly in Western populations with high rates of obesity and metabolic syndrome. NASH-related cirrhosis typically demonstrates a more indolent progression compared to viral or alcoholic aetiologies, though the eventual development of decompensation carries similar mortality risks. The association between NASH and cardiovascular disease creates additional complexity in prognostication, as cardiac events frequently contribute to mortality in this patient population.
Recent epidemiological data suggests that NASH-related end-stage liver disease carries 5-year survival rates of approximately 60-70% following initial decompensation, though these figures vary considerably based on patient demographics and comorbidity burden. The rising prevalence of NASH cirrhosis has significant implications for liver transplant allocation, as this population tends to be older with multiple cardiovascular risk factors that may influence transplant candidacy.
Hepatitis C Virus-Related decompensated cirrhosis prognosis
The advent of direct-acting antiviral agents has revolutionised the natural history of hepatitis C virus-related liver disease, offering the possibility of viral cure even in patients with established cirrhosis. However, patients with decompensated HCV cirrhosis who achieve sustained virological response still face elevated mortality risks compared to the general population. The degree of hepatic fibrosis regression following viral eradication varies substantially, with some patients experiencing meaningful improvement whilst others demonstrate minimal histological changes.
Survival outcomes for decompensated HCV cirrhosis depend heavily on the timing of antiviral intervention relative to the development of complications. Patients achieving viral cure prior to decompensation demonstrate significantly improved outcomes, whilst those treated after developing ascites or encephalopathy show more modest survival benefits. The presence of hepatocellular carcinoma in HCV-related cirrhosis further complicates prognostication, requiring integrated oncological and hepatological management approaches.
Primary biliary cholangitis terminal phase life expectancy
Primary biliary cholangitis represents a unique autoimmune liver condition with distinctive progression patterns and survival characteristics. The disease typically affects middle-aged women and progresses slowly over decades before reaching end-stage manifestations. Patients with primary biliary cholangitis who develop decompensated cirrhosis often experience concurrent complications including severe pruritus, bone disease, and malabsorption syndromes that significantly impact quality of life.
Terminal phase primary biliary cholangitis carries survival estimates of 12-24 months following initial decompensation, though individual variation remains considerable. The response to ursodeoxycholic acid treatment influences long-term outcomes, with biochemical responders demonstrating significantly improved survival compared to non-responders. Early diagnosis and prompt therapeutic intervention remain crucial factors in optimising long-term outcomes for patients with this progressive autoimmune condition.
Wilson’s disease fulminant hepatic failure survival statistics
Wilson’s disease presents unique challenges in end-stage liver disease management due to its potential for both acute fulminant presentation and chronic progressive cirrhosis. Fulminant Wilson’s disease carries extraordinarily high mortality rates, approaching 80-90% without emergency liver transplantation. The combination of severe hepatic dysfunction, neurological manifestations, and psychiatric symptoms creates complex management scenarios requiring multidisciplinary expertise.
The Wilson’s disease prognostic index provides valuable guidance for transplant decision-making, incorporating serum bilirubin levels, international normalised ratio, white blood cell count, and serum albumin concentration. Patients with high prognostic scores require urgent transplant evaluation, as survival without hepatic replacement approaches zero in fulminant cases. Early recognition of Wilson’s disease presentation remains critical, as delayed diagnosis significantly worsens survival outcomes.
Complications-based mortality risk stratification
The development of specific complications in end-stage liver disease serves as powerful predictors of mortality risk, often superseding underlying disease aetiology in prognostic significance. These complications represent manifestations of portal hypertension, hepatocellular dysfunction, and systemic inflammatory responses that characterise advanced hepatic failure. Understanding the individual and cumulative impact of these complications enables more precise survival estimation and guides therapeutic priorities.
Variceal bleeding recurrence and survival impact
Oesophageal and gastric variceal bleeding represents one of the most immediately life-threatening complications of portal hypertension, with initial bleeding episodes carrying mortality rates of 15-20% and rebleeding events approaching 60% mortality within six weeks if left untreated. The development of variceal haemorrhage fundamentally alters the natural history of cirrhosis, transitioning patients from compensated to decompensated states with dramatically reduced survival expectations.
Contemporary management strategies including endoscopic band ligation, sclerotherapy, and prophylactic beta-blockade have improved short-term survival outcomes, though long-term prognosis remains guarded. Patients who experience variceal bleeding demonstrate 1-year survival rates of approximately 60-70%, declining to 35-50% at five years. The size and location of varices, presence of concurrent hepatic encephalopathy, and response to endoscopic therapy all influence individual survival outcomes.
Secondary prevention strategies play crucial roles in improving long-term survival following variceal bleeding episodes. The combination of endoscopic variceal ligation and non-selective beta-blockers reduces rebleeding rates by approximately 40-50% compared to either intervention alone. Prophylactic measures remain essential for optimising survival outcomes in patients with established portal hypertension and variceal disease.
Spontaneous bacterial peritonitis mortality rates
Spontaneous bacterial peritonitis represents a serious infectious complication occurring in 15-25% of hospitalised cirrhotic patients with ascites, carrying significant mortality implications despite advances in antibiotic therapy. The condition develops due to bacterial translocation from the intestinal tract combined with impaired immune responses characteristic of advanced liver disease. Early recognition and prompt antibiotic administration remain critical factors influencing survival outcomes.
Hospital mortality rates for spontaneous bacterial peritonitis range from 20-40%, with one-year survival rates approaching 30-50% depending on underlying hepatic function and presence of concurrent complications. The development of antibiotic-resistant organisms has complicated treatment approaches, requiring broader spectrum antimicrobial coverage and contributing to increased mortality risks. Patients surviving initial episodes face elevated risks for recurrent infections, necessitating antibiotic prophylaxis strategies.
The presence of spontaneous bacterial peritonitis fundamentally alters the trajectory of end-stage liver disease, representing a sentinel event that signals advanced immune dysfunction and poor overall prognosis.
Hepatic encephalopathy grade IV prognostic indicators
Grade IV hepatic encephalopathy represents the most severe manifestation of neurocognitive dysfunction in end-stage liver disease, characterised by coma and complete loss of consciousness. This complication develops in approximately 45% of cirrhotic patients and carries mortality rates approaching 80% within one year of first occurrence. The pathophysiology involves accumulation of neurotoxic substances, particularly ammonia, coupled with alterations in neurotransmitter metabolism and cerebral blood flow.
Survival outcomes for Grade IV hepatic encephalopathy depend heavily on precipitating factors, underlying hepatic reserve, and response to therapeutic interventions. Patients with reversible precipitants such as gastrointestinal bleeding or infection demonstrate better outcomes compared to those with spontaneous encephalopathy development. The presence of cerebral oedema significantly worsens prognosis, requiring intensive care management and consideration of intracranial pressure monitoring.
Portal Hypertension-Related ascites survival outcomes
The development of ascites marks a critical transition in the natural history of cirrhosis, reducing median survival from more than 10 years to approximately 2-4 years. Refractory ascites, defined as ascites unresponsive to maximal diuretic therapy or recurring rapidly after large-volume paracentesis, carries even worse prognostic implications with median survival of 6-12 months. The presence of ascites reflects advanced portal hypertension and hepatic synthetic dysfunction that fundamentally alters disease trajectory.
Management strategies for ascites significantly influence survival outcomes, with patients responding well to diuretic therapy demonstrating improved prognosis compared to those requiring frequent paracentesis procedures. The development of complications such as spontaneous bacterial peritonitis or hepatorenal syndrome further deteriorates survival expectations. Early recognition and aggressive management of ascites remain crucial for optimising patient outcomes and quality of life in advanced liver disease.
Liver transplantation candidacy and waitlist mortality
Liver transplantation represents the definitive treatment for end-stage liver disease, offering the possibility of long-term survival and improved quality of life for carefully selected patients. However, the scarcity of donor organs coupled with stringent selection criteria means that many patients with advanced hepatic dysfunction may not qualify for transplantation or may deteriorate whilst awaiting organ availability. Understanding transplant candidacy requirements and waitlist dynamics becomes essential for patients and families navigating end-stage liver disease.
The evaluation process for liver transplantation involves comprehensive assessment of medical, psychological, and social factors that influence post-transplant outcomes. Candidates must demonstrate adequate cardiac and pulmonary reserve, absence of active substance abuse, and realistic expectations regarding post-transplant care requirements. Age limitations vary between transplant centres, though most programmes consider patients up to 65-70 years old for standard criteria organs. The presence of hepatocellular carcinoma within specific size and number criteria may qualify patients for transplantation, though recurrence risks must be carefully balanced.
Waitlist mortality represents a significant challenge in liver transplantation, with approximately 10-15% of listed patients dying annually whilst awaiting organ availability. The MELD-based allocation system prioritises patients based on disease severity, though even high-priority candidates may experience prolonged waiting periods due to blood type compatibility, body size matching, and geographic considerations. Recent data indicates that patients with MELD scores above 35 face 6-month waitlist mortality rates exceeding 25%, highlighting the urgent need for increased donor organ availability.
The concept of waitlist mortality encompasses both direct liver-related deaths and mortality from complications arising during the waiting period. Patients may develop hepatocellular carcinoma progression, cardiovascular events, or infectious complications that render them unsuitable for transplantation. Regular monitoring and proactive management of waitlist candidates remains essential for maintaining transplant eligibility and optimising post-transplant outcomes.
Alternative approaches including living donor liver transplantation offer potential solutions for reducing waitlist mortality, though donor availability remains limited. Split liver transplantation techniques enable one deceased donor organ to benefit two recipients, though technical complexity and size matching requirements limit widespread application. The development of machine perfusion technologies may expand the utilisation of marginal donor organs, potentially reducing waitlist times for suitable candidates.
Palliative care integration in terminal hepatic disease management
Palliative care principles have gained increasing recognition as essential components of comprehensive end-stage liver disease management, addressing the complex physical, psychological, and spiritual needs of patients facing terminal diagnoses. The integration of palliative approaches alongside disease-modifying treatments provides holistic support that significantly improves quality of life whilst respecting patient autonomy and dignity. Research demonstrates that early palliative care involvement reduces symptom burden, decreases hospital admissions, and improves patient satisfaction scores compared to traditional medical management alone.
The symptom burden in end-stage liver disease can be overwhelming, with patients experiencing multiple concurrent complications including intractable pruritus, severe fatigue, pain, and cognitive dysfunction. Palliative care specialists possess expertise in symptom management techniques that complement hepatological interventions, offering multimodal approaches to address complex symptomatology. The judicious use of opioid medications requires careful consideration due to altered drug metabolism in hepatic dysfunction, necessitating dose adjustments and alternative analgesic strategies.
Psychosocial support represents a critical component of palliative care integration, addressing the profound emotional distress experienced by patients and families confronting terminal liver disease. The uncertainty surrounding transplant candidacy and waitlist outcomes creates unique psychological challenges requiring specialised intervention approaches. Advance care planning discussions enable patients to articulate their values and preferences regarding end-of-life care, ensuring that medical interventions align with individual goals and beliefs.
Family education and support services play vital roles in palliative care integration, helping caregivers understand disease progression whilst providing practical guidance for home management of complex symptoms. The burden on family caregivers can be substantial, with many experiencing depression, anxiety, and physical exhaustion related to their caregiving responsibilities. Support groups, respite care services, and educational resources help families navigate the challenges of caring for loved ones with terminal liver disease.
The integration of palliative care principles transforms the approach to end-stage liver disease from purely life-sustaining interventions to comprehensive care that honours patient dignity whilst maximising comfort and quality of remaining life.
Contemporary treatment interventions affecting life expectancy outcomes
Recent advances in hepatic medicine have introduced novel therapeutic interventions that may modestly improve survival outcomes for patients with end-stage liver disease, though the impact on overall prognosis remains limited without definitive transplantation. These contemporary approaches focus on managing specific complications, optimising nutritional status, and potentially slowing disease progression through targeted interventions. The development of artificial liver support systems represents an emerging frontier that may provide bridging therapy for transplant candidates or temporary support during acute decompensation episodes.
Molecular adsorbent recirculating system (MARS) therapy offers extracorporeal liver support through albumin dialysis, removing protein-bound toxins that accumulate in hepatic failure. Clinical trials suggest that MARS treatment may improve survival in acute-on-chronic liver failure patients, though the technology remains expensive and technically complex. Similar artificial liver support systems including single-pass albumin dialysis and fractionated plasma separation show promise for managing specific complications of end-stage liver disease.
Nutritional interventions have gained recognition as critical components of comprehensive end-stage liver disease management, with protein-energy malnutrition present in 50-90% of cirrhotic patients. Branched-chain amino acid supplementation may improve muscle mass and potentially enhance survival outcomes, whilst zinc replacement addresses common deficiencies that impair immune function. The optimisation of nutritional status requires individualised approaches considering altered metabolism, malabsorption syndromes, and dietary restrictions related to ascites management.
Emerging pharmacological interventions target specific pathophysiological mechanisms underlying hepatic decompensation and complications. Albumin infusion protocols extend beyond simple volume expansion, potentially offering anti-inflammatory and detoxification benefits that improve outcomes in spontaneous bacterial peritonitis and hepatorenal syndrome. Novel vasopressin analogues show promise for managing hepatorenal syndrome with improved efficacy compared to traditional approaches, though availability remains limited in many healthcare systems.
The role of antimicrobial prophylaxis continues to evolve, with selective intestinal decontamination strategies potentially reducing bacterial translocation and infection rates in high-risk cirrhotic patients. However, concerns regarding antibiotic resistance development require careful consideration when implementing prophylactic protocols. Individualised risk-benefit assessments guide decision-making regarding prophylactic interventions, balancing infection prevention against potential adverse consequences.
Regenerative medicine approaches including stem cell therapies represent experimental interventions that may eventually impact end-stage liver disease outcomes, though current evidence remains preliminary. Hepatocyte transplantation offers theoretical advantages over whole organ transplantation, potentially addressing donor shortage issues whilst providing targeted hepatic support. The translation of regenerative approaches from experimental protocols to clinical applications requires extensive safety and efficacy validation through rigorous clinical trial processes.
Psychopharmacological interventions addressing depression, anxiety, and cognitive dysfunction in end-stage liver disease patients may indirectly influence survival outcomes through improved treatment adherence and quality of life measures. The complex interactions between psychiatric medications and altered hepatic metabolism necessitate careful dose adjustments and monitoring protocols. Multidisciplinary approaches incorporating psychiatric expertise enhance comprehensive care delivery whilst addressing the profound psychological burden of terminal liver disease diagnosis.