Neural foraminal stenosis represents one of the most clinically significant yet frequently misunderstood conditions encountered in spinal imaging. When the small openings between vertebrae narrow, compressing nerve roots as they exit the spinal canal, the resulting pathology can manifest as debilitating radicular symptoms that profoundly impact quality of life. Understanding the meaning of neural foraminal stenosis on MRI requires a comprehensive appreciation of both the anatomical complexities and the sophisticated imaging techniques employed in modern diagnostic protocols.
This condition affects millions of individuals worldwide, with prevalence rates increasing substantially with age. By the sixth decade of life, approximately 40% of the population demonstrates some degree of foraminal narrowing on imaging studies, though remarkably, only 17.5% of those with severe stenosis experience symptomatic radiculopathy. The disconnect between anatomical findings and clinical presentation underscores the critical importance of correlating MRI findings with patient symptoms and physical examination findings.
Anatomical foundation of neural foraminal stenosis: vertebral architecture and pathophysiology
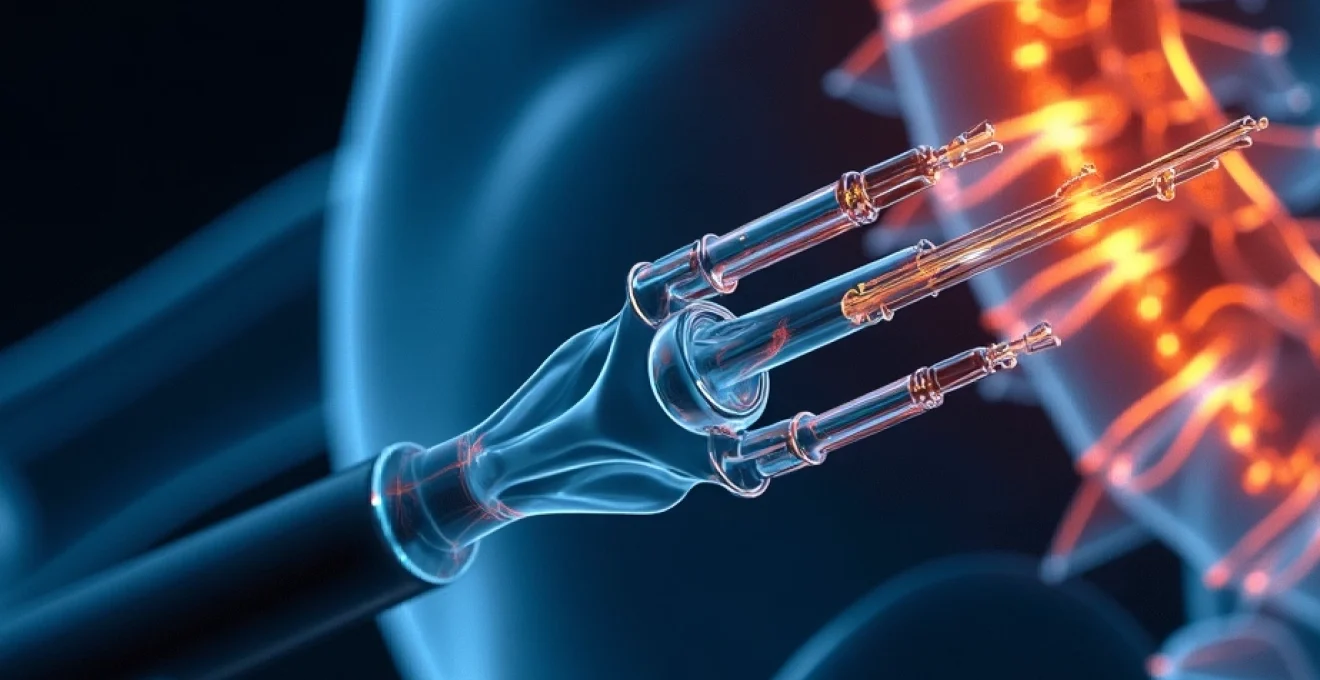
The neural foramen, also termed the intervertebral foramen, represents a critical anatomical structure that serves as the exit pathway for spinal nerve roots as they branch from the central spinal cord. These openings are bounded by specific anatomical landmarks that can become compromised through various pathological processes. Anteriorly, the foramen is bordered by the posterior aspect of the vertebral body and the intervertebral disc. The superior and inferior boundaries are formed by the pedicles of adjacent vertebrae, whilst the posterior border consists of the facet joints and ligamentum flavum.
Understanding the three-dimensional architecture of the neural foramen is fundamental to interpreting MRI findings, as pathological changes in any of these bounding structures can contribute to foraminal narrowing and subsequent nerve root compression.
The pathophysiology of neural foraminal stenosis involves a complex interplay of degenerative processes that affect multiple anatomical structures simultaneously. As the spine ages, several concurrent processes contribute to foraminal narrowing, including disc height loss, facet joint arthropathy, ligamentous hypertrophy, and osteophyte formation. These changes create a cascade effect where the loss of disc height reduces the vertical dimension of the foramen, whilst concurrent facet joint hypertrophy and ligamentous thickening compromise the anteroposterior diameter.
Intervertebral foramen dimensions and normal morphometric parameters
Normal foraminal dimensions vary significantly based on spinal level and individual anatomical variations. In the cervical spine, the typical foraminal height ranges from 10-12mm, with an anteroposterior diameter of 6-8mm. Lumbar foramina are generally larger, measuring 15-20mm in height and 8-12mm in anteroposterior dimension. These measurements provide crucial reference points for determining the degree of stenosis present on imaging studies.
The morphology of the neural foramen follows a characteristic funnel shape, with the narrowest point typically occurring at the level of the pedicles. This anatomical configuration means that even modest degrees of swelling or structural changes can result in significant nerve root compression. Understanding these normal parameters allows radiologists and clinicians to accurately assess the severity of foraminal compromise and predict the likelihood of symptomatic radiculopathy.
Facet joint hypertrophy and ligamentum flavum thickening mechanisms
Facet joint hypertrophy represents one of the primary mechanisms contributing to neural foraminal stenosis, particularly affecting the posterior and lateral aspects of the foramen. As the articular cartilage degenerates within the facet joints, compensatory bone formation occurs, resulting in osteophyte development and joint capsule thickening. This process directly encroaches upon the neural foramen, reducing the available space for nerve root passage.
The ligamentum flavum undergoes predictable age-related changes that contribute significantly to foraminal narrowing. Normal ligamentum flavum thickness measures approximately 2-3mm, but with advancing age and degenerative processes, this can increase to 5-8mm or more. The thickened ligament not only reduces foraminal space but also loses its elastic properties, becoming more rigid and less able to accommodate normal spinal movements without compressing neural structures.
Disc herniation patterns: posterolateral and Far-Lateral protrusions
Disc herniations affecting the neural foramen follow specific anatomical patterns that determine their clinical significance. Posterolateral herniations typically compress the traversing nerve root within the lateral recess before it enters the foramen, whilst far-lateral herniations directly impact the exiting nerve root within the foramen itself. These distinct patterns produce different clinical syndromes and require tailored therapeutic approaches.
Far-lateral disc herniations, also termed extraforaminal herniations, represent approximately 10% of all lumbar disc herniations but often present diagnostic challenges due to their location outside the spinal canal. These herniations are particularly problematic because they compress the nerve root at its most vulnerable point, where it lacks the protective covering of cerebrospinal fluid and is most susceptible to inflammatory mediators released from the herniated disc material.
Spondylolisthesis impact on foraminal diameter reduction
Spondylolisthesis, characterised by the forward slippage of one vertebra relative to the one below, creates a unique pattern of foraminal compromise that differs from other degenerative processes. The forward displacement reduces both the height and anteroposterior diameter of the neural foramen, creating a characteristic “fish-mouth” appearance on sagittal imaging sequences. This geometric alteration can result in severe nerve root compression even with relatively modest degrees of vertebral displacement.
The severity of foraminal stenosis in spondylolisthesis correlates directly with the degree of vertebral slippage, with Grade II slippages (25-50% displacement) typically producing significant foraminal compromise. However, the clinical impact also depends on the rate of progression, with acute slippages more likely to produce symptomatic radiculopathy than chronic, slowly progressive cases where the nerve roots may adapt to gradual compression.
MRI signal characteristics and diagnostic criteria for neural foraminal stenosis
Modern MRI protocols for evaluating neural foraminal stenosis employ multiple imaging sequences designed to optimally visualise both the bony and soft tissue components contributing to foraminal narrowing. The diagnostic accuracy of MRI in detecting clinically significant foraminal stenosis approaches 85-90% when appropriate sequences and imaging planes are utilised. However, the interpretation of foraminal stenosis requires careful attention to technical factors, including patient positioning, sequence selection, and understanding of normal anatomical variations.
The assessment of neural foraminal stenosis on MRI involves evaluating several key parameters, including the degree of foraminal narrowing, the presence of nerve root compression, signal changes within the nerve root itself, and associated inflammatory changes. These findings must be interpreted within the context of the patient’s clinical presentation, as asymptomatic foraminal stenosis is remarkably common, particularly in older individuals. The challenge lies in distinguishing between incidental imaging findings and clinically relevant pathology.
T1-weighted and T2-Weighted imaging protocols for foraminal assessment
T1-weighted sequences provide excellent anatomical detail of the bony structures surrounding the neural foramen, allowing clear delineation of the pedicles, facet joints, and vertebral body margins. The normal neural foramen appears as a well-defined opening filled with epidural fat, which demonstrates high signal intensity on T1-weighted images. When foraminal stenosis is present, this fat signal is reduced or obliterated, replaced by lower signal intensity soft tissue or bone.
T2-weighted sequences complement T1-weighted imaging by providing superior contrast between neural tissue and surrounding structures. The nerve roots typically demonstrate intermediate signal intensity on T2-weighted images, whilst cerebrospinal fluid appears bright. Inflammatory changes associated with nerve root compression often manifest as increased T2 signal intensity around the affected nerve root, though this finding is not always present even in symptomatic cases.
Fat-suppressed sequences: STIR and T2 Fat-Sat applications
Fat-suppressed sequences, including Short Tau Inversion Recovery (STIR) and T2 fat-saturated images, play a crucial role in detecting subtle inflammatory changes associated with neural foraminal stenosis. These sequences suppress the signal from epidural fat, making it easier to identify oedema and inflammatory changes within and around compressed nerve roots. STIR sequences are particularly valuable as they are less susceptible to magnetic field inhomogeneities that can affect fat saturation techniques.
The application of fat-suppressed sequences has revealed that nerve root oedema and enhancement are more common than previously recognised, occurring in approximately 30% of patients with symptomatic foraminal stenosis. These inflammatory changes may persist for weeks to months after the initial compression, potentially explaining why some patients experience prolonged symptoms even after successful decompressive procedures.
Oblique sagittal plane imaging: optimising foraminal visualisation
Oblique sagittal imaging represents a significant advancement in foraminal stenosis assessment, allowing direct visualisation of the neural foramen in its optimal imaging plane. Traditional axial and sagittal images often provide suboptimal foraminal assessment due to the oblique orientation of the neural foramen relative to these standard imaging planes. Oblique sagittal images are acquired parallel to the long axis of the neural foramen, providing unparalleled visualisation of foraminal anatomy and pathology.
The technique involves angling the imaging plane approximately 45-60 degrees to the sagittal plane, depending on the spinal level and individual anatomy. This approach allows direct measurement of foraminal dimensions and provides clear visualisation of the relationship between nerve roots and surrounding structures. Studies have demonstrated that oblique sagittal imaging increases diagnostic confidence in foraminal stenosis assessment by approximately 25% compared to standard imaging planes alone.
Grading systems: wildermuth classification and lee grading scale
Several standardised grading systems have been developed to quantify the severity of neural foraminal stenosis and improve inter-observer agreement among radiologists. The Wildermuth classification system, one of the most widely adopted approaches, categorises foraminal stenosis into four grades based on the degree of epidural fat obliteration and nerve root compression visible on MRI.
The Lee grading scale provides an alternative approach, focusing on the cross-sectional area of the neural foramen and the degree of nerve root compression. This system demonstrates excellent correlation with surgical findings and has proven valuable in predicting the likelihood of successful conservative management versus the need for surgical intervention. Both grading systems have shown good inter-observer reliability when applied by experienced musculoskeletal radiologists.
Spinal Level-Specific neural foraminal stenosis patterns
Neural foraminal stenosis presents distinct patterns and characteristics depending on the spinal level affected, with each region demonstrating unique anatomical considerations and clinical presentations. Cervical foraminal stenosis typically affects the C5-C6 and C6-C7 levels most commonly, correlating with the areas of greatest cervical spine mobility and mechanical stress. The cervical neural foramina are naturally smaller than their lumbar counterparts, making them more susceptible to compromise from relatively minor degenerative changes.
Lumbar foraminal stenosis most frequently occurs at the L4-L5 and L5-S1 levels, corresponding to the areas of maximum load-bearing and rotational stress in the lower spine. The lumbar neural foramina demonstrate unique anatomical features, including a more pronounced lateral component that can be affected by far-lateral disc herniations and facet joint hypertrophy. The L5-S1 level presents particular challenges due to the transitional anatomy and the presence of the sacral promontory, which can contribute to foraminal compromise.
Thoracic foraminal stenosis, whilst less common than cervical or lumbar involvement, presents unique diagnostic challenges due to the smaller size of the thoracic neural foramina and the presence of the rib articulations. The thoracic spine’s relative stability means that foraminal stenosis at these levels is more often related to specific pathological processes such as disc herniation or tumour involvement rather than routine degenerative changes. When thoracic foraminal stenosis does occur, it often produces distinctive clinical presentations including intercostal neuralgia and referred pain patterns that can mimic cardiac or pulmonary pathology.
The clinical significance of foraminal stenosis varies dramatically by spinal level, with cervical stenosis more likely to produce motor symptoms due to the mixed motor and sensory nature of cervical nerve roots, whilst lumbar stenosis typically manifests primarily as sensory symptoms and radicular pain.
Advanced MRI techniques: 3T imaging and constructive interference in steady state
The advent of 3T MRI systems has revolutionised the assessment of neural foraminal stenosis by providing superior spatial resolution and signal-to-noise ratios compared to conventional 1.5T systems. The increased field strength allows for thinner slice acquisitions and improved visualisation of small anatomical structures, including individual nerve rootlets and subtle pathological changes within the neural foramen. Advanced 3T protocols can achieve spatial resolutions of 0.5mm or less, enabling detection of early foraminal stenosis that might be missed on lower field strength systems.
Constructive Interference in Steady State (CISS) sequences represent a significant technological advancement in neural imaging, providing exquisite detail of cerebrospinal fluid and neural structures. These sequences demonstrate the nerve roots and their relationship to surrounding cerebrospinal fluid with remarkable clarity, allowing detection of subtle nerve root compression and displacement that may not be apparent on conventional sequences. CISS imaging has proven particularly valuable in cases where conventional MRI findings are equivocal but clinical suspicion for foraminal stenosis remains high.
Diffusion tensor imaging (DTI) represents an emerging technique for evaluating nerve root integrity and function in patients with foraminal stenosis. This advanced MRI technique can detect microstructural changes within compressed nerve roots before conventional imaging abnormalities become apparent. Early studies suggest that DTI parameters may serve as biomarkers for nerve root injury and could potentially predict which patients are most likely to benefit from surgical intervention.
Differential diagnosis: distinguishing foraminal stenosis from radicular pathologies
The differential diagnosis of neural foraminal stenosis encompasses a broad spectrum of conditions that can produce similar clinical presentations and imaging findings. Piriformis syndrome, a common cause of sciatic-type symptoms, can closely mimic lumbar foraminal stenosis, particularly when affecting the L5 or S1 nerve roots. The key distinguishing feature lies in the anatomical location of nerve compression, with piriformis syndrome affecting the nerve root more distally as it passes through the piriformis muscle rather than at the level of the neural foramen.
Peripheral neuropathies, including diabetic neuropathy and vitamin B12 deficiency, can produce radicular-type symptoms that may be confused with foraminal stenosis. However, these conditions typically demonstrate a more diffuse, symmetrical distribution of symptoms and lack the specific dermatomal patterns characteristic of nerve root compression. Advanced electrodiagnostic studies, including nerve conduction studies and electromyography, can help differentiate between central (foraminal) and peripheral causes of radiculopathy.
Spinal tumours, both primary and metastatic, represent important considerations in the differential diagnosis of foraminal stenosis, particularly when symptoms are progressive or associated with constitutional symptoms such as weight loss or night pain. MRI with gadolinium contrast is essential for detecting neoplastic processes, as tumours typically demonstrate characteristic enhancement patterns that differ from the non-enhancing degenerative changes seen in typical foraminal stenosis. The presence of bone destruction or pathological fractures should raise immediate suspicion for malignant involvement.
Clinical correlation: MRI findings and symptom presentation in radiculopathy syndromes
The correlation between MRI findings and clinical symptoms in neural foraminal stenosis remains one of the most challenging aspects of spinal imaging interpretation. Studies consistently demonstrate that the severity of anatomical stenosis on MRI does not always correlate directly with symptom severity or functional impairment. This discordance highlights the importance of comprehensive clinical evaluation and the need to consider multiple factors beyond pure anatomical narrowing when determining treatment recommendations.
Research has identified several MRI findings that demonstrate stronger correlations with symptomatic radiculopathy, including the presence of nerve root oedema or enhancement, complete obliteration of epidural fat around the nerve root, and evidence of nerve root displacement or deformation. These findings, when present in conjunction with appropriate clinical symptoms, provide stronger evidence for clinically significant foraminal stenosis than measurements of foraminal dimensions alone.
The development of machine learning algorithms for automated foraminal stenosis detection represents another promising advancement in spinal imaging. These artificial intelligence systems can analyze multiple MRI sequences simultaneously, identifying subtle patterns that may escape human detection. Early pilot studies suggest that AI-assisted interpretation can improve diagnostic accuracy by up to 15% whilst significantly reducing interpretation time for radiologists.
Functional MRI techniques, including dynamic imaging during flexion and extension movements, provide valuable insights into the behavior of foraminal stenosis under physiological conditions. Some patients demonstrate significant changes in foraminal dimensions with spinal positioning, explaining why symptoms may be position-dependent. This dynamic assessment can be particularly valuable in surgical planning, helping identify patients who may benefit from motion-preserving procedures versus those requiring fusion techniques.
The integration of advanced MRI techniques with clinical assessment represents the future of foraminal stenosis evaluation, moving beyond static anatomical assessment toward functional and predictive imaging approaches.
Quantitative MRI metrics, including T2 relaxometry and magnetization transfer imaging, are emerging as potential biomarkers for nerve root health and compression severity. These techniques can detect biochemical changes within compressed nerve roots before structural abnormalities become apparent on conventional imaging. Research suggests that these quantitative measures may better predict treatment outcomes and help identify patients at risk for progressive neurological deterioration.
The prognostic value of specific MRI findings continues to evolve as our understanding of foraminal stenosis pathophysiology advances. Nerve root displacement, measured as the deviation from the central axis of the neural foramen, has emerged as a particularly strong predictor of symptomatic radiculopathy. When nerve root displacement exceeds 2mm from the foraminal center, the likelihood of symptomatic presentation increases dramatically, providing valuable guidance for treatment decision-making.
Contemporary imaging protocols increasingly emphasize the importance of assessing inflammatory markers around compressed nerve roots. The presence of perineural enhancement on post-contrast imaging or increased T2 signal intensity in the epidural space correlates strongly with acute symptom onset and may predict better response to anti-inflammatory treatments. These findings can guide clinicians toward more targeted therapeutic approaches, potentially avoiding unnecessary surgical interventions in selected patients.
The temporal evolution of foraminal stenosis on serial MRI examinations provides crucial insights into disease progression and treatment response. Studies tracking patients over multiple years reveal that approximately 30% of individuals with mild stenosis progress to moderate or severe narrowing, whilst 15% actually demonstrate improvement, likely related to decreased inflammatory components or adaptive remodeling processes. This natural history data is invaluable for counseling patients about prognosis and treatment expectations.
Multi-parametric imaging approaches, combining anatomical and functional MRI techniques, represent the cutting edge of foraminal stenosis assessment. These comprehensive protocols can evaluate nerve root morphology, signal characteristics, enhancement patterns, and functional integrity within a single examination. The integration of multiple imaging biomarkers improves diagnostic confidence and provides a more complete picture of disease severity and progression risk.
The role of artificial intelligence in foraminal stenosis imaging continues to expand, with deep learning algorithms now capable of automatically measuring foraminal dimensions, detecting nerve root compression, and even predicting treatment outcomes based on imaging patterns. These tools hold particular promise for standardizing assessments across different institutions and reducing inter-observer variability that has historically complicated foraminal stenosis research and clinical care.