Hair colouring has become an integral part of modern beauty routines, with millions of individuals worldwide regularly using hair dyes to enhance their appearance. However, beneath the glossy marketing promises lies a concerning reality: chemical hair dyes can cause significant scalp irritation, leading to painful scabs and long-term skin damage. These adverse reactions stem from potent chemical formulations designed to penetrate hair shafts, but which can equally damage delicate scalp tissue.
The scalp’s unique anatomy makes it particularly vulnerable to chemical assault. Unlike other areas of skin, the scalp contains dense networks of hair follicles, sebaceous glands, and blood vessels, creating multiple pathways for chemical penetration. When hair dye ingredients breach the skin’s protective barrier, they trigger inflammatory cascades that can result in blistering, crusting, and ultimately, scab formation. Understanding these mechanisms becomes crucial for anyone experiencing post-dyeing scalp complications.
Chemical allergens in hair dye formulations causing scalp irritation
Modern hair dyes contain complex chemical formulations designed to achieve lasting colour transformation, but these same ingredients can wreak havoc on sensitive scalp tissue. The concentration and combination of these chemicals determine both the effectiveness of the colouring process and the likelihood of adverse reactions. Professional-grade formulations often contain higher concentrations of active ingredients, increasing both efficacy and risk profiles.
The chemistry behind hair dyeing involves opening the hair cuticle, depositing colour molecules, and sealing the result. This process requires aggressive chemical agents that can inadvertently damage surrounding skin tissue. Chemical sensitivity varies significantly among individuals , with some people developing severe reactions to concentrations that others tolerate without incident. Genetic predisposition, previous chemical exposure, and existing skin conditions all influence individual susceptibility levels.
Para-phenylenediamine (PPD) sensitivity and contact dermatitis mechanisms
Para-phenylenediamine represents the most notorious culprit in hair dye allergic reactions, present in approximately 75% of permanent hair colouring products. This aromatic amine compound creates durable colour bonds but simultaneously acts as a potent sensitising agent. PPD sensitivity develops through repeated exposure, with initial applications potentially causing no symptoms while subsequent uses trigger increasingly severe reactions.
The molecular structure of PPD allows it to penetrate skin barriers efficiently, binding to skin proteins and creating hapten-protein complexes. These complexes are recognised as foreign substances by the immune system, triggering Type IV delayed hypersensitivity reactions. Once sensitisation occurs, even trace amounts of PPD can provoke severe inflammatory responses , including vesicle formation, extensive erythema, and eventual scab development as lesions heal.
Ammonia and hydrogen peroxide alkaline burns on scalp tissue
Ammonia serves as the primary alkalising agent in many hair dye formulations, raising hair shaft pH to facilitate cuticle opening and colour penetration. However, this same alkalising action can cause significant chemical burns when in contact with scalp tissue. Ammonia concentrations in hair dyes typically range from 1-6%, with professional products often containing higher levels that increase burn risk exponentially.
Hydrogen peroxide functions as both a bleaching agent and colour developer, with concentrations varying from 3% in consumer products to 12% in professional formulations. The oxidising action of hydrogen peroxide can cause immediate tissue damage, resulting in protein denaturation and cellular membrane disruption. Combined with ammonia, these chemicals create a synergistic effect that amplifies tissue damage potential , often resulting in deep chemical burns that heal with significant scab formation.
Resorcinol and toluene-2,5-diamine allergic reactions
Resorcinol functions as a colour coupler in many hair dye formulations, particularly those producing brown and auburn shades. This phenolic compound can cause both irritant and allergic contact dermatitis, with cross-reactivity patterns extending to other phenolic substances found in cosmetics and industrial applications. Individuals sensitised to resorcinol often develop reactions to related compounds, complicating future product selection and use.
Toluene-2,5-diamine, commonly used in semi-permanent and temporary hair colours, presents similar allergenicity profiles to PPD but with distinct immunological characteristics. Studies indicate that approximately 15% of individuals with confirmed PPD sensitivity also react to toluene-2,5-diamine, suggesting shared antigenic properties. The delayed onset of these allergic reactions often leads to continued exposure and worsening of symptoms , as users may not immediately connect their scalp irritation to recent hair colouring activities.
Methylchloroisothiazolinone Preservative-Induced inflammation
Preservatives in hair dye formulations, particularly methylchloroisothiazolinone (MCI), serve essential functions in preventing microbial contamination but can trigger significant allergic responses in sensitive individuals. MCI sensitivity has increased dramatically over recent years, with some European studies reporting sensitisation rates approaching 4% in tested populations. This preservative can cause particularly severe contact dermatitis, often resulting in widespread scalp inflammation and subsequent scab formation.
The inflammatory response to MCI typically manifests as acute contact dermatitis with marked oedema, vesiculation, and intense pruritus.
The combination of mechanical trauma from scratching and chemical irritation from continued exposure creates optimal conditions for secondary bacterial infection and prolonged healing times.
Recovery often involves extensive scab formation as the damaged epidermis attempts to restore barrier function.
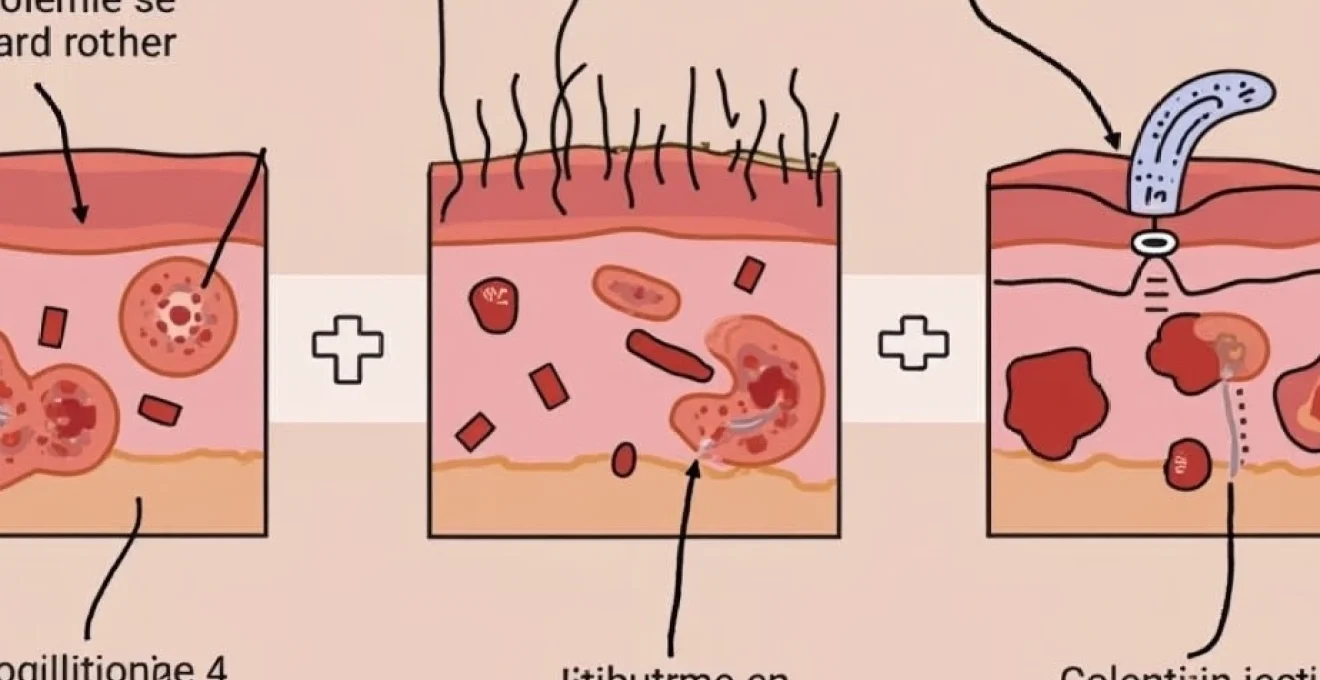
Pathophysiology of scalp scab formation following hair colouring
The formation of scabs on the scalp following hair dye application represents a complex pathophysiological process involving multiple cellular and molecular mechanisms. Understanding this process helps explain why some individuals develop minor irritation while others experience severe, scarring reactions. The scalp’s unique anatomical features, including its rich vascularisation and dense follicular structure, influence both the severity of initial damage and subsequent healing patterns.
Chemical hair dyes disrupt normal scalp homeostasis through direct cytotoxic effects and immune-mediated inflammatory responses. The severity of tissue damage depends on numerous factors, including chemical concentration, contact duration, skin barrier integrity, and individual susceptibility. Once tissue damage occurs, the body initiates a predictable cascade of inflammatory and reparative processes that ultimately determine whether healing occurs without complication or results in significant scab formation and potential scarring.
Epidermal barrier disruption and inflammatory cascade response
The scalp’s stratum corneum normally provides effective protection against chemical penetration, but hair dye alkalising agents can rapidly compromise this barrier. Ammonia and other alkaline substances increase skin pH from its normal acidic range (4.5-5.5) to alkaline levels (8-9), causing corneocyte swelling and intercellular lipid disruption. This barrier compromise allows deeper penetration of other chemical components, amplifying tissue damage potential.
Once barrier disruption occurs, keratinocytes release inflammatory mediators including interleukin-1α, interleukin-8, and tumour necrosis factor-α. These cytokines initiate a complex inflammatory cascade involving neutrophil recruitment, mast cell degranulation, and complement activation. The resulting inflammatory response can persist for days or weeks , even after chemical removal, contributing to prolonged tissue damage and delayed healing processes that favour scab formation over normal epithelial repair.
Keratinocyte damage and secondary bacterial infection risk
Chemical hair dyes cause direct keratinocyte damage through protein denaturation, membrane disruption, and mitochondrial dysfunction. Severely damaged keratinocytes undergo apoptosis or necrosis, creating areas of denuded epidermis that are highly susceptible to bacterial colonisation. The warm, moist environment beneath developing scabs provides ideal conditions for bacterial proliferation, particularly Staphylococcus aureus and Streptococcus pyogenes.
Secondary bacterial infection significantly complicates the healing process, often transforming minor chemical irritation into serious soft tissue infection. Bacterial toxins and enzymes further damage surrounding healthy tissue, expanding the area of injury and promoting more extensive scab formation.
Studies indicate that secondary bacterial infection occurs in approximately 30% of severe chemical burns, significantly prolonging healing times and increasing scarring risk.
Early recognition and treatment of secondary infection becomes crucial for optimal outcomes.
Histamine release and localised oedema development
Allergic reactions to hair dye components trigger massive histamine release from mast cells and basophils, causing characteristic symptoms of redness, swelling, and intense itching. Histamine increases vascular permeability, allowing protein-rich fluid to leak into surrounding tissues and creating the marked oedema commonly observed in severe hair dye reactions. This fluid accumulation stretches the skin, causing pain and contributing to tissue damage through mechanical stress.
The intense pruritus associated with histamine release often leads to vigorous scratching, which mechanically damages already compromised skin. Scratching can introduce bacteria from under fingernails directly into damaged tissue , significantly increasing secondary infection risk. The combination of chemical damage, mechanical trauma from scratching, and bacterial contamination creates optimal conditions for extensive scab formation and potential permanent scarring.
Wound healing phases and crusting formation timeline
Scalp scab formation follows predictable phases of wound healing, beginning with hemostasis and inflammation, progressing through proliferation, and concluding with remodelling. In chemical burns from hair dye, the inflammatory phase is often prolonged due to continued chemical irritation and immune system activation. This extended inflammation delays the transition to proliferative healing, resulting in more extensive scab formation than would occur with simple mechanical injuries.
The proliferative phase involves fibroblast activation, collagen synthesis, and angiogenesis, processes that can be significantly impaired by chemical damage to dermal structures. When normal proliferative healing is compromised, the body compensates by forming thicker, more extensive scabs that may persist for weeks or months. The final remodelling phase determines whether healing occurs with normal skin architecture or results in permanent scarring and altered pigmentation.
Clinical assessment of chemical burns and allergic contact dermatitis
Accurate clinical assessment of hair dye-related scalp injuries requires systematic evaluation of both the extent of tissue damage and the underlying pathophysiological mechanisms. Healthcare providers must differentiate between irritant contact dermatitis, allergic contact dermatitis, and chemical burns, as treatment approaches vary significantly among these conditions. The assessment process involves detailed history-taking, physical examination, and often specialised testing to determine the specific causative agents and appropriate therapeutic interventions.
Physical examination should document the distribution, severity, and characteristics of scalp lesions, paying particular attention to areas of confluent erythema, vesiculation, and scab formation. The pattern of involvement often provides crucial clues about the underlying pathophysiology , with well-demarcated areas suggesting direct chemical contact versus diffuse involvement indicating systemic allergic responses. Photographic documentation proves valuable for monitoring healing progress and assessing treatment efficacy over time.
Laboratory investigations may include patch testing to identify specific allergens, bacterial cultures if secondary infection is suspected, and occasionally skin biopsy for histopathological confirmation of diagnosis. Patch testing should be delayed until acute inflammation subsides, typically 4-6 weeks after the initial reaction, to avoid false-positive results and potential exacerbation of existing lesions.
Proper timing of diagnostic testing can mean the difference between accurate allergen identification and misleading results that compromise future treatment planning.
Evidence-based treatment protocols for hair Dye-Related scalp lesions
Effective treatment of hair dye-related scalp injuries requires a multifaceted approach addressing both the immediate inflammatory response and long-term healing optimisation. The therapeutic strategy must be tailored to the specific type and severity of injury, with careful consideration of potential complications such as secondary bacterial infection and scarring. Early intervention significantly improves outcomes, emphasising the importance of prompt medical evaluation following severe hair dye reactions.
Treatment protocols should follow a systematic approach, beginning with immediate decontamination and symptomatic relief, progressing through active treatment of inflammation and infection, and concluding with measures to optimise healing and prevent complications. The complexity of chemical burns often requires multidisciplinary care involving dermatologists, wound care specialists, and occasionally plastic surgeons for severe cases with significant scarring potential.
Topical corticosteroid application techniques and potency selection
Topical corticosteroids represent the cornerstone of anti-inflammatory treatment for hair dye-related contact dermatitis and chemical burns. Potency selection depends on lesion severity, with mild reactions responding to low-potency preparations (hydrocortisone 1-2.5%) while severe cases may require super-high potency formulations (clobetasol propionate 0.05%). Application technique significantly influences therapeutic efficacy, with thin, even distribution providing optimal drug penetration while minimising systemic absorption risk.
Duration of corticosteroid treatment typically ranges from 1-4 weeks, with gradual tapering to prevent rebound inflammation. Prolonged use of high-potency corticosteroids on facial and scalp areas can cause skin atrophy, telangiectasia, and other adverse effects , necessitating careful monitoring and appropriate treatment modification. Alternative anti-inflammatory agents, such as calcineurin inhibitors (tacrolimus, pimecrolimus), may provide effective treatment with reduced side effect profiles for sensitive areas.
Antimicrobial therapy for secondary staphylococcal infections
Secondary bacterial infection complicates approximately 30% of severe chemical burns, with Staphylococcus aureus being the most common pathogen. Early recognition of infection is crucial, as delayed treatment can result in deeper tissue involvement, increased scarring, and systemic complications. Clinical signs of secondary infection include increased pain, purulent discharge, expanding erythema, and formation of thick, adherent scabs with surrounding cellulitis.
Topical antimicrobial therapy suffices for superficial infections, with mupirocin 2% ointment being the first-line treatment due to its excellent staphylococcal coverage and minimal resistance patterns. Severe or extensive infections require systemic antibiotic therapy, with oral flucloxacillin or erythromycin being appropriate first-line choices pending culture results.
The emergence of methicillin-resistant Staphylococcus aureus (MRSA) in community-acquired infections has complicated treatment decisions, sometimes necessitating more aggressive antibiotic regimens from the outset.
Emollient barrier repair using Ceramide-Based formulations
Restoration of the epidermal barrier represents a critical component of healing optimisation following chemical injury. Ceramide-based emollients have demonstrated superior efficacy in barrier repair compared to traditional petrolatum-based products, providing both immediate symptom relief and long-term healing enhancement. These formulations should be applied 2-3 times daily to affected areas, with particular attention to maintaining adequate hydration during the scab formation and healing phases.
Advanced barrier repair formulations containing ceramides, hyaluronic acid, and niacinamide offer synergistic benefits for damaged scalp tissue. Regular application of these specialised emollients can reduce healing time by 30-40% compared to standard wound care approaches, while simultaneously minimising the risk of permanent scarring and hyperpigmentation. Patient education regarding proper application techniques and expected healing timelines improves treatment adherence and outcomes.
Cool compress therapy and scalp cooling methods
Cool compress therapy provides immediate symptomatic relief while helping to limit inflammatory damage in acute hair dye reactions. Application of cool, damp cloths for 15-20 minutes every 2-3 hours during the first 48-72 hours can significantly reduce pain, swelling, and tissue damage progression. The cooling effect causes vasoconstriction, reducing inflammatory mediator delivery to affected tissues and limiting the extent of chemical burn injury.
Specialised scalp cooling devices, originally developed for chemotherapy-induced alopecia prevention, have shown promise in managing severe chemical burns. These devices maintain precise temperature control while ensuring uniform cooling distribution across the entire scalp surface. Professional cooling therapy may prevent deep tissue damage and reduce the likelihood of permanent scarring in severe cases, though access to such specialised equipment may be limited outside major medical centres.
Professional salon safety protocols and patch testing procedures
Professional salons bear significant responsibility for preventing hair dye-related injuries through implementation of comprehensive safety protocols and mandatory patch testing procedures. Industry standards require detailed client consultation, thor
ough skin assessment, allergy history documentation, and appropriate product selection based on individual risk factors. Salons must establish clear protocols for recognising early signs of adverse reactions and implementing immediate intervention strategies when complications arise.
Mandatory continuing education programs ensure that salon professionals remain current with evolving safety standards and new product formulations. Professional liability depends heavily on adherence to established safety protocols, with documentation of proper procedures serving as crucial protection against potential legal complications. Comprehensive client records, including detailed consultation notes and patch test results, provide essential evidence of professional care standards.
Patch testing represents the gold standard for preventing severe allergic reactions to hair dye components. Professional protocols require patch testing at least 48-72 hours before any new colour application, with careful observation for signs of sensitivity during this period. The test involves applying small amounts of the intended hair dye mixture to clean skin behind the ear or on the inner elbow, covering with a protective patch, and monitoring for reactions.
Industry studies indicate that proper patch testing can prevent up to 95% of severe allergic reactions, making it an indispensable component of professional hair colouring services.
Advanced patch testing protocols may include testing multiple product components separately to identify specific allergens, allowing for more targeted product selection and customised formulations. Digital photography of test sites enables accurate documentation and comparison over time, improving the reliability of sensitivity assessments and providing valuable records for future reference.
Long-term scalp recovery and scarring prevention strategies
Long-term recovery from hair dye-related scalp injuries requires comprehensive management addressing both physical healing and psychological impacts. The recovery process can extend from weeks to months, depending on injury severity, individual healing capacity, and adherence to treatment protocols. Early intervention significantly influences long-term outcomes, with prompt, appropriate treatment dramatically reducing the likelihood of permanent scarring and pigmentation changes.
Scarring prevention strategies must begin immediately following injury recognition, as the window for optimal intervention is relatively narrow. Once mature scar tissue forms, therapeutic options become significantly more limited and expensive, emphasising the critical importance of early, aggressive intervention to preserve normal scalp anatomy and function.
Nutritional support plays a crucial role in optimising healing outcomes, with adequate protein intake, vitamin C, zinc, and essential fatty acids being particularly important for tissue repair processes. Hydration maintenance, stress management, and sleep optimisation further support the body’s natural healing mechanisms, creating optimal conditions for recovery without complications.
Silicone-based scar prevention products have demonstrated significant efficacy when applied during the early healing phases, typically beginning once initial scab formation occurs. These products maintain optimal moisture levels while providing mechanical protection against trauma, creating ideal conditions for ordered collagen synthesis and normal tissue architecture restoration.
Regular follow-up appointments with dermatology specialists ensure appropriate healing progression monitoring and early intervention if complications develop. Professional assessment can identify subtle signs of abnormal healing patterns that might escape patient recognition, allowing for prompt treatment modifications to prevent adverse outcomes.
Research indicates that patients receiving structured, professional follow-up care experience 60% fewer complications and significantly better cosmetic outcomes compared to those managing recovery independently.
For severe cases with established scarring, advanced treatment options may include laser therapy, microneedling, corticosteroid injections, or surgical revision procedures. These interventions require careful patient selection and realistic expectation management, as complete restoration to pre-injury appearance may not always be achievable despite optimal treatment approaches.
Psychological support becomes particularly important for individuals experiencing visible scarring or permanent appearance changes following hair dye injuries. The emotional impact of disfiguring injuries can be substantial, potentially affecting self-esteem, social relationships, and overall quality of life. Professional counselling services specialising in appearance-related trauma can provide valuable support during the recovery process.
Prevention of future reactions requires permanent avoidance of identified allergens, careful product selection, and potentially genetic testing for individuals with strong family histories of chemical sensitivities. Cross-reactivity patterns mean that avoiding only the specific product that caused the initial reaction may be insufficient, necessitating broader restrictions on chemically-related hair care products and cosmetics.
Alternative hair colouring methods, including natural plant-based dyes, temporary colour products, and professional techniques using hypoallergenic formulations, may provide satisfactory cosmetic results for individuals with established sensitivities. However, even these alternatives require careful evaluation and patch testing, as cross-reactivity and unexpected sensitivities can occur with any topically applied product.
Long-term scalp health maintenance involves gentle cleansing routines, regular moisturisation with barrier-repair products, sun protection, and ongoing monitoring for signs of sensitivity to new products or environmental exposures. Patients should be educated about recognising early warning signs of adverse reactions, enabling prompt intervention before severe complications develop.
Documentation of sensitivity patterns, effective treatments, and recovery timelines creates valuable medical records that inform future care decisions and help prevent repeat injuries. This information becomes particularly crucial if emergency treatment is required, allowing healthcare providers to quickly understand the patient’s history and implement appropriate interventions without delay.