The detection of small amounts of free fluid in the cul-de-sac during ultrasound examinations represents one of the most common findings in pelvic imaging, yet it continues to generate uncertainty among both patients and healthcare providers. This fluid accumulation in the pouch of Douglas, the most dependent portion of the peritoneal cavity, can range from entirely physiological to pathologically significant. Understanding the distinction between normal and abnormal fluid collections requires comprehensive knowledge of pelvic anatomy, ultrasound detection techniques, and the clinical context in which these findings occur. The significance of small free fluid varies considerably depending on factors such as the patient’s menstrual cycle phase, symptoms, and concurrent medical conditions.
Anatomical structure of the pouch of douglas and physiological free fluid
Rectovesical pouch anatomy in male patients
In male anatomy, the rectovesical pouch represents the most dependent portion of the peritoneal cavity, situated between the rectum posteriorly and the bladder anteriorly. This anatomical configuration creates a natural collection point for peritoneal fluid, making it the primary location for detecting free fluid in male patients. The pouch extends approximately 7.5 centimetres below the level of the peritoneal reflection, creating a substantial space where even small amounts of fluid can accumulate and become radiographically apparent.
The anatomical boundaries of the rectovesical pouch are formed by the peritoneal reflections from the posterior bladder wall to the anterior rectal wall. Understanding these landmarks is crucial for accurate ultrasound interpretation, as the depth and configuration of this space can vary significantly between individuals based on factors such as age, body habitus, and previous surgical interventions.
Rectouterine pouch configuration in female patients
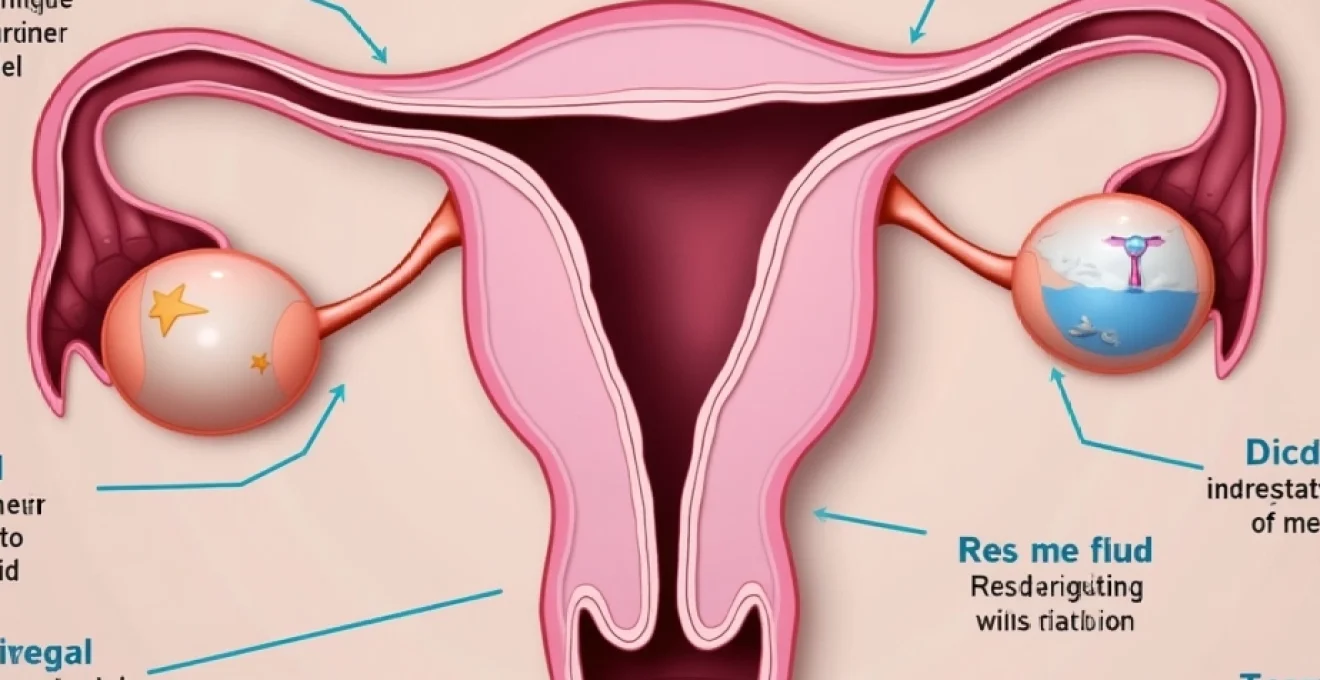
The female pelvic anatomy presents a more complex configuration with the rectouterine pouch, also known as the pouch of Douglas or posterior cul-de-sac, representing the deepest part of the peritoneal cavity. This space lies between the posterior aspect of the uterus and cervix anteriorly and the rectum posteriorly. The presence of the uterus and adnexal structures creates additional anatomical variations that can influence fluid distribution patterns.
In reproductive-age women, the rectouterine pouch typically measures between 5-9 centimetres in depth, though this can vary significantly based on uterine position, pelvic organ prolapse, and previous surgical history. The anatomical relationship between the ovaries and the pouch of Douglas is particularly important, as ovarian processes frequently result in fluid accumulation in this dependent portion of the pelvis.
Normal physiological fluid accumulation mechanisms
Physiological free fluid in the cul-de-sac occurs through several normal mechanisms that maintain peritoneal homeostasis. The peritoneum produces approximately 50-100 millilitres of fluid daily through normal metabolic processes, with this fluid serving as a lubricant for visceral movement and nutrient transport. This physiological fluid is typically reabsorbed through lymphatic drainage at a rate that maintains equilibrium under normal circumstances.
During the menstrual cycle, additional physiological fluid accumulation occurs, particularly around ovulation when follicular rupture releases fluid into the peritoneal cavity. This cyclical fluid production can result in small amounts of free fluid being detected on ultrasound examinations, particularly during the mid-cycle period. The volume of this physiological fluid rarely exceeds 20-30 millilitres and typically appears anechoic on ultrasound examination.
Gravity-dependent fluid distribution patterns
The distribution of free fluid within the pelvis follows predictable gravity-dependent patterns that are essential for accurate interpretation of imaging findings. When patients are upright, fluid naturally gravitates to the most dependent portions of the peritoneal cavity, primarily the pouch of Douglas in females and the rectovesical pouch in males. However, patient positioning during ultrasound examination can significantly influence the apparent location and quantity of detectable fluid.
Understanding these distribution patterns becomes particularly important when differentiating between small amounts of physiological fluid and pathological collections. Pathological fluid collections often demonstrate different distribution patterns and may be associated with loculations, septations, or debris that distinguishes them from normal physiological fluid.
Ultrasound detection techniques for minimal pelvic free fluid
Transvaginal sonography optimisation for Cul-de-Sac visualisation
Transvaginal ultrasound represents the gold standard for detecting small amounts of free fluid in the female pelvis, offering superior resolution and proximity to target structures compared to transabdominal approaches. The technique requires systematic evaluation of the pouch of Douglas using both sagittal and transverse scanning planes to accurately assess fluid quantity and characteristics. Optimal visualisation requires appropriate gain settings and frequency selection to differentiate between minimal free fluid and normal pelvic structures.
The transvaginal approach allows detection of fluid volumes as small as 5-10 millilitres, significantly lower than the threshold for transabdominal detection. This enhanced sensitivity makes transvaginal ultrasound particularly valuable for identifying early pathological processes or monitoring changes in fluid accumulation over time. The close proximity of the transvaginal probe to pelvic structures also enables better characterisation of fluid echogenicity and associated findings.
Transabdominal scanning protocol modifications
While transvaginal ultrasound offers superior sensitivity, transabdominal scanning remains important for comprehensive pelvic assessment and may be the only option in certain clinical scenarios. Optimising transabdominal techniques for free fluid detection requires attention to bladder filling, patient positioning, and probe selection. A moderately filled bladder provides an acoustic window while avoiding overdistension that could compress pelvic structures and obscure small fluid collections.
The use of lower frequency transducers (2-5 MHz) in transabdominal scanning provides adequate penetration while maintaining reasonable axial resolution for fluid detection. Systematic scanning through the pelvis in multiple planes ensures comprehensive assessment of potential fluid collection sites, including paracolic gutters and other dependent portions of the peritoneal cavity.
Doppler assessment of fluid characteristics
Doppler ultrasound techniques can provide additional information about the nature of detected free fluid, particularly when differentiating between simple fluid and more complex collections. Power Doppler and colour Doppler can identify vascular flow within septations or debris, suggesting inflammatory or malignant processes. The absence of internal vascularity supports the diagnosis of simple physiological fluid or uncomplicated pathological collections.
Advanced Doppler techniques, including spectral analysis of detected flow patterns, can further characterise complex fluid collections. High-resistance flow patterns may suggest inflammatory processes, while low-resistance flow could indicate malignant involvement. However, the interpretation of Doppler findings must always be correlated with clinical context and other imaging characteristics.
Quantitative measurement standards using linear probes
Accurate quantification of free fluid requires standardised measurement techniques that can be reproduced across different operators and institutions. The most commonly used method involves measuring the maximum anterior-posterior diameter of the fluid collection in the sagittal plane, with measurements typically recorded in millimetres. Collections measuring less than 20mm in maximum diameter are generally considered small and may represent physiological fluid in appropriate clinical contexts.
Three-dimensional ultrasound techniques offer the potential for more accurate volume calculations of free fluid collections, though these methods are not yet widely standardised in clinical practice. The use of automated measurement tools and standardised imaging protocols can improve consistency in fluid quantification and facilitate meaningful comparison between serial examinations.
Clinical significance of small volume free fluid detection
The clinical significance of small amounts of free fluid in the cul-de-sac depends heavily on the clinical context in which it is detected. In asymptomatic patients undergoing routine pelvic ultrasound, small amounts of anechoic free fluid may represent normal physiological findings, particularly during certain phases of the menstrual cycle. However, the same finding in a patient presenting with acute pelvic pain requires careful evaluation for underlying pathological processes.
Research indicates that approximately 15-20% of reproductive-age women demonstrate small amounts of free fluid on routine pelvic ultrasound examinations. This baseline prevalence underscores the importance of correlating imaging findings with clinical symptoms and examination findings. The timing of the ultrasound examination in relation to the menstrual cycle can significantly influence the likelihood of detecting physiological free fluid.
The quantity of free fluid alone is not sufficient to determine clinical significance , as small amounts of pathological fluid may be associated with serious conditions such as ectopic pregnancy or ovarian torsion. Conversely, larger amounts of physiological fluid may accumulate in certain circumstances without indicating underlying pathology. The key lies in comprehensive assessment that includes fluid characteristics, associated findings, and clinical correlation.
Serial monitoring of free fluid collections can provide valuable information about their clinical significance. Physiological fluid collections typically demonstrate stability or gradual resolution over time, while pathological collections may show progressive increase in volume or development of complex characteristics. This temporal evolution can help guide clinical decision-making and determine the need for further intervention.
Pathological conditions associated with Cul-de-Sac fluid accumulation
Ovarian cyst rupture and haemorrhagic corpus luteum
Ovarian cyst rupture represents one of the most common causes of pathological free fluid accumulation in reproductive-age women. Functional cysts, including follicular cysts and corpus luteum cysts, may rupture spontaneously or following trauma, releasing cyst contents into the peritoneal cavity. The volume of fluid released can vary significantly, from small amounts that may be clinically silent to larger volumes causing significant pelvic pain and distension.
Haemorrhagic corpus luteum cysts deserve particular attention as they can produce both echogenic and anechoic free fluid depending on the degree of haemorrhage and the time elapsed since rupture. Fresh haemorrhage may appear echogenic on ultrasound, while older haemorrhage or serous fluid appears anechoic. The clinical presentation typically includes sudden onset of unilateral pelvic pain that may be severe initially but gradually improves over 24-48 hours.
The ultrasound appearance of free fluid from ovarian cyst rupture may include internal echoes, layering effects, or septations depending on the nature of the cyst contents. Complex cysts containing dermoid elements or endometriotic material may produce particularly characteristic appearances when ruptured. The key to diagnosis lies in identifying the source of the free fluid through careful evaluation of both ovaries and correlation with the patient’s clinical presentation.
Pelvic inflammatory disease manifestations
Pelvic inflammatory disease (PID) can cause free fluid accumulation through several mechanisms, including increased capillary permeability, inflammatory exudation, and tubo-ovarian abscess formation. The free fluid associated with PID is typically complex, containing inflammatory cells, debris, and potentially infected material. This complex fluid may demonstrate internal echoes, septations, or layering effects that distinguish it from simple physiological fluid.
The clinical presentation of PID with associated free fluid typically includes pelvic pain, fever, and abnormal vaginal discharge. Laboratory findings may reveal elevated white blood cell count and inflammatory markers. The ultrasound examination may demonstrate thickened fallopian tubes, complex adnexal masses, and free fluid with complex characteristics. The combination of clinical, laboratory, and imaging findings is essential for accurate diagnosis.
Chronic PID can result in adhesion formation and loculated fluid collections that may persist long after the acute infectious process has resolved. These chronic changes can create complex pelvic anatomy with multiple small fluid collections separated by adhesions. Understanding this progression is important for interpreting imaging findings in patients with a history of pelvic inflammatory disease.
Endometriosis-related fluid collections
Endometriosis frequently involves the pouch of Douglas and can cause both acute and chronic free fluid accumulation. Active endometriotic lesions may produce inflammatory fluid, while endometriotic cysts (endometriomas) can rupture and release thick, chocolate-coloured fluid into the peritoneal cavity. This endometriotic fluid often has characteristic ultrasound appearances, including ground-glass echogenicity and resistance to gravity-dependent layering.
The cyclical nature of endometriosis means that free fluid accumulation may vary with the menstrual cycle, typically being most prominent during menstruation when endometriotic deposits are most active. Patients with deep infiltrating endometriosis affecting the pouch of Douglas may develop complex adhesive disease that creates loculated fluid collections and distorted pelvic anatomy.
Culdocentesis, though rarely performed in modern practice, was historically used to diagnose endometriosis by analysing free fluid for the presence of endometrial cells and haemosiderin-laden macrophages. While transvaginal ultrasound has largely replaced this diagnostic approach, understanding the historical context helps appreciate the significance of free fluid findings in patients with suspected endometriosis.
Tubal pregnancy complications and free fluid
Ectopic pregnancy, particularly tubal pregnancy, represents a potentially life-threatening cause of free fluid in the cul-de-sac. The presence of free fluid in a patient with a positive pregnancy test and pelvic pain should raise immediate suspicion for ectopic pregnancy with tubal rupture or leakage. Even small amounts of free fluid in this clinical context warrant urgent evaluation and close monitoring.
The characteristics of free fluid from ectopic pregnancy can vary from anechoic to highly echogenic, depending on the degree of haemorrhage and the time elapsed since bleeding began. Fresh haemorrhage may appear echogenic and may demonstrate layering or clot formation within the dependent portions of the pelvis. The volume of free fluid can range from minimal to massive, with larger volumes generally indicating more significant haemorrhage and greater clinical urgency.
Serial monitoring of free fluid volume in suspected ectopic pregnancy provides valuable information about ongoing bleeding and helps guide clinical management decisions. Increasing volumes of free fluid, particularly when accompanied by clinical deterioration, may indicate progressive haemorrhage requiring surgical intervention. The absence of free fluid does not exclude ectopic pregnancy , as unruptured ectopic pregnancies may not produce detectable fluid accumulation.
Differential diagnosis framework for physiological versus pathological fluid
Developing a systematic approach to differentiating physiological from pathological free fluid requires careful consideration of multiple factors including patient demographics, clinical presentation, timing in relation to menstrual cycle, and imaging characteristics. The integration of these factors provides a framework for clinical decision-making that balances the need for appropriate investigation with the avoidance of unnecessary interventions.
Patient age represents a significant factor in the differential diagnosis, as physiological free fluid is most commonly seen in reproductive-age women, particularly around ovulation. Postmenopausal women have lower baseline rates of physiological fluid production, making any detected free fluid more likely to represent underlying pathology. Similarly, prepubertal girls rarely demonstrate physiological free fluid, and any fluid accumulation in this population warrants careful investigation.
The timing of ultrasound examination in relation to the menstrual cycle significantly influences the probability of detecting physiological free fluid, with peak accumulation typically occurring around mid-cycle during ovulation.
Clinical symptoms provide crucial context for interpreting free fluid findings. Asymptomatic patients with small amounts of anechoic free fluid are more likely to have physiological accumulations, while patients presenting with acute pelvic pain, fever, or abnormal bleeding require careful evaluation for underlying pathological processes. The severity and character of symptoms should be correlated with the volume and characteristics of detected free fluid.
Imaging characteristics of the free fluid itself offer important diagnostic clues. Physiological fluid is typically anechoic, mobile, and conforms to dependent portions of the pelvis without septations or debris. Pathological fluid collections may demonstrate internal echoes, septations, loculations, or associated inflammatory changes in surrounding tissues. The presence of organised clot or debris within the fluid strongly suggests an underlying pathological process.
Laboratory investigations can provide additional diagnostic information, particularly in cases where the clinical significance of free fluid remains uncertain. Elevated inflammatory markers, abnormal complete blood counts, or positive pregnancy tests can help clarify the underlying aetiology and guide appropriate management decisions. The combination of clinical, imaging, and laboratory findings provides the most reliable framework for distinguishing physiological from pathological free fluid.
Management protocols and Follow-Up recommendations for detected free fluid
The management of patients with detected free fluid in the cul-de-sac requires individualised approaches based on clinical context, fluid characteristics, and associated findings. For asymp
tomatic patients with small amounts of anechoic free fluid detected incidentally during routine pelvic ultrasound, initial management typically involves observation with clinical correlation. These patients should be reassured about the likely physiological nature of their findings while being educated about symptoms that would warrant immediate medical attention.
For patients presenting with acute pelvic symptoms and associated free fluid, the management approach depends on the clinical severity and suspected underlying aetiology. Patients with signs of haemodynamic instability require immediate surgical consultation and may need emergency intervention regardless of the volume of detected free fluid. Stable patients can often be managed with close observation, serial examinations, and follow-up imaging studies.
Serial ultrasound monitoring represents a valuable tool for assessing the evolution of free fluid collections over time. Physiological fluid collections typically demonstrate stability or gradual resolution over 24-72 hours, while pathological collections may show progressive increase or development of complex characteristics. The timing of follow-up imaging should be individualised based on clinical presentation, with more frequent monitoring for symptomatic patients or those with concerning initial findings.
Pain management protocols for patients with free fluid-related symptoms should focus on appropriate analgesia while maintaining diagnostic clarity. Non-steroidal anti-inflammatory drugs (NSAIDs) can be effective for managing inflammatory pain associated with conditions such as ovarian cyst rupture or mild pelvic inflammatory disease. However, caution must be exercised in patients with suspected ectopic pregnancy or other conditions where bleeding risk may be increased.
Antibiotic therapy may be indicated when free fluid is associated with suspected infectious processes such as pelvic inflammatory disease or tubo-ovarian abscess. The choice of antibiotic regimen should be based on local resistance patterns and guideline recommendations, with consideration for both aerobic and anaerobic coverage in pelvic infections. Close monitoring of clinical response to antibiotic therapy is essential, as failure to improve may indicate the need for surgical intervention or alternative diagnoses.
Patient education plays a crucial role in the management of detected free fluid, particularly for those with likely physiological findings. Patients should be informed about the normal occurrence of small amounts of pelvic fluid, especially during certain phases of the menstrual cycle. Clear instructions should be provided regarding symptoms that warrant immediate medical attention, including severe pelvic pain, heavy bleeding, fever, or signs of systemic illness.
Documentation standards for free fluid findings should include detailed descriptions of fluid volume, echogenicity, location, and associated findings. Standardised reporting templates can improve consistency across different practitioners and institutions while ensuring that relevant clinical information is communicated effectively to referring physicians. The use of structured reporting systems also facilitates quality assurance and research activities related to pelvic free fluid detection.
Follow-up recommendations for patients with detected free fluid should be tailored to the individual clinical scenario and suspected underlying aetiology. Asymptomatic patients with small amounts of likely physiological fluid may require only routine gynaecological follow-up, while those with pathological fluid collections may need specialist referral and more intensive monitoring. Clear communication between radiologists, clinicians, and patients is essential for ensuring appropriate follow-up care and preventing unnecessary anxiety or delayed diagnosis.
Risk stratification frameworks can help guide management decisions by categorising patients based on their likelihood of having significant underlying pathology. Low-risk patients include asymptomatic individuals with small amounts of anechoic free fluid detected during routine screening, while high-risk patients encompass those with acute symptoms, complex fluid characteristics, or concerning clinical presentations. This stratification approach helps optimise resource utilisation while ensuring appropriate care for all patients.
Quality improvement initiatives focused on free fluid detection and management can help standardise care delivery and improve patient outcomes. These initiatives might include development of clinical pathways, implementation of structured reporting systems, and establishment of metrics for tracking diagnostic accuracy and patient satisfaction. Regular review of cases can identify opportunities for improvement and ensure that current best practices are being followed consistently across the healthcare system.