The discovery of white substances coating pubic hair can understandably cause concern and confusion. This phenomenon, whilst often alarming upon first observation, typically stems from natural physiological processes or treatable medical conditions. Understanding the various causes behind white deposits on pubic hair enables individuals to make informed decisions about their health and seek appropriate treatment when necessary. From natural sebaceous secretions to fungal infections, bacterial overgrowth, and parasitic infestations, multiple factors can contribute to this common yet poorly understood occurrence. The intimate nature of the affected area often prevents open discussion, leaving many to wonder about the significance of these white coatings and whether medical intervention is required.
Sebaceous gland secretions and natural keratin deposits
The pubic region contains numerous sebaceous glands that naturally produce sebum, an oily substance designed to lubricate and protect hair shafts and surrounding skin. These microscopic structures work continuously to maintain the health of hair follicles, but their activity can sometimes result in visible white or cream-coloured deposits along the hair shaft. Understanding how these natural processes function helps distinguish between normal physiological responses and potential health concerns requiring medical attention.
Sebum overproduction in pubic hair follicles
Excessive sebum production represents one of the most common causes of white substance accumulation on pubic hair. The sebaceous glands in the genital area are particularly active due to the high concentration of androgen receptors in this region. When these glands produce more oil than can be naturally dispersed, the excess sebum crystallises and adheres to hair shafts, creating visible white or yellowish deposits. This overproduction often correlates with hormonal fluctuations, stress levels, and individual genetic predispositions. The waxy consistency of accumulated sebum can trap dead skin cells and environmental particles, further contributing to the white appearance and potentially creating an ideal environment for bacterial colonisation.
Keratinous plugs formation in terminal hair shafts
Keratin, the structural protein that forms the foundation of hair, skin, and nails, can occasionally form plugs within hair follicles and along hair shafts. These keratinous deposits appear as small, white, granular substances that feel gritty to the touch and may cause hair to become brittle or prone to breakage. The formation process typically involves the accumulation of dead skin cells that fail to shed naturally, instead clumping together around the hair shaft. Environmental factors such as humidity, friction from clothing, and inadequate hygiene can exacerbate this condition. Unlike sebaceous deposits, keratinous plugs tend to be harder and more difficult to remove, often requiring gentle exfoliation or professional treatment to prevent damage to the underlying hair follicle.
Apocrine gland dysfunction and white residue accumulation
The pubic region contains a high density of apocrine sweat glands, which differ significantly from the eccrine glands found elsewhere on the body. These specialised glands produce a protein-rich secretion that, when broken down by skin bacteria, can create white, chalky residues on hair shafts. Apocrine gland dysfunction, often triggered by hormonal imbalances, stress, or certain medications, can lead to altered secretion composition and increased residue formation. The resulting deposits may have a distinctive odour and can be particularly noticeable in individuals with coarse or curly pubic hair. This condition often improves with proper hygiene practices and may benefit from antiperspirant products specifically designed for sensitive areas.
Hormonal fluctuations affecting sebaceous output
Hormonal changes throughout the menstrual cycle, during pregnancy, menopause, or due to endocrine disorders can dramatically impact sebaceous gland activity in the pubic region. Elevated androgen levels, in particular, stimulate increased oil production, leading to more pronounced white deposits on hair shafts. These hormonal influences can also affect the composition of sebaceous secretions, making them more likely to solidify and adhere to hair. Women may notice cyclical patterns in white substance formation, with increased deposits occurring during specific phases of their menstrual cycle. Understanding these patterns can help distinguish between normal hormonal variations and underlying medical conditions requiring professional evaluation.
Fungal infections causing white coating on pubic hair
Fungal infections represent a significant category of conditions that can produce white substances on pubic hair. The warm, moist environment of the genital region provides optimal conditions for various fungal species to proliferate, leading to characteristic white coatings, flakes, or nodular deposits along hair shafts. These infections often develop gradually and may be accompanied by additional symptoms such as itching, burning, or unusual odours. Early recognition and appropriate treatment are essential to prevent complications and reduce transmission risk to partners.
Candida albicans overgrowth and hyphal formation
Candida albicans, the fungus responsible for thrush, can occasionally extend beyond its typical vaginal or penile locations to affect pubic hair. When this yeast transitions from its normal single-cell form to its pathogenic hyphal state, it produces white, cottage cheese-like deposits that can coat hair shafts. This transformation typically occurs when the natural balance of microorganisms is disrupted by factors such as antibiotic use, diabetes, compromised immune function, or excessive moisture retention. The resulting white substance often has a characteristic sweet or musty odour and may be accompanied by intense itching. Treatment requires antifungal medications and addressing underlying predisposing factors to prevent recurrence.
Tinea cruris manifestations in pubic region
Tinea cruris, commonly known as jock itch, occasionally extends into the pubic hair region, producing distinctive white scaling and flaking that adheres to hair shafts. This dermatophyte infection creates a white, powdery substance composed of fungal elements and dead skin cells. The infection typically begins in the groin folds and may spread to involve pubic hair, particularly in cases of poor hygiene, excessive sweating, or tight-fitting clothing. The white deposits associated with tinea cruris often have a distinctive ring-like pattern and may be accompanied by redness, scaling, and intense itching. Topical antifungal treatments are usually effective, though severe cases may require oral medication.
Malassezia furfur colonisation and white scale production
Malassezia furfur, a lipophilic yeast naturally present on human skin, can sometimes overgrow in the pubic region, particularly in individuals with oily skin or those using occlusive personal care products. This overgrowth produces fine, white scales that adhere to hair shafts and surrounding skin. The condition is often exacerbated by hot, humid weather conditions and may be more prevalent in individuals with certain genetic predispositions. The white scaling associated with Malassezia overgrowth is typically finer and more easily removed than deposits from other fungal infections. Treatment involves antifungal shampoos or topical medications containing selenium sulphide, ketoconazole, or zinc pyrithione.
Trichosporon species infection patterns
Trichosporon species cause white piedra, a superficial fungal infection characterised by the formation of soft, white nodules that loosely attach to hair shafts. These nodules, composed of fungal elements and debris, can easily be removed but tend to recur without proper treatment. White piedra typically affects individuals in tropical or subtropical climates and may be associated with poor hygiene, excessive hair oiling, or bathing in contaminated water sources. The condition primarily affects the hair shaft rather than the follicle, making it distinct from other fungal infections. Complete hair removal from the affected area provides the most effective treatment, though topical antifungal agents can be used when shaving is not acceptable.
Bacterial biofilm formation and metabolic byproducts
Bacterial colonisation of pubic hair can lead to the formation of complex biofilms and the production of white, chalky metabolic byproducts that coat hair shafts. These bacterial communities, predominantly composed of Corynebacterium species and other gram-positive bacteria, thrive in the warm, moist environment of the pubic region. The biofilms they produce serve as protective matrices that allow bacteria to adhere strongly to hair surfaces while producing various compounds that can appear as white, cream-coloured, or yellowish deposits.
Trichomycosis axillaris, despite its misleading name suggesting a fungal origin, is actually a bacterial condition caused by Corynebacterium species overgrowth. When this condition affects pubic hair—known as trichomycosis pubis—it produces distinctive white, yellow, or reddish nodular concretions along hair shafts. These deposits consist of tightly packed bacterial colonies and their metabolic products, creating a characteristic gritty texture that differs significantly from fungal infections or natural sebaceous accumulations.
The bacterial metabolisation of apocrine sweat components contributes significantly to both the formation of white deposits and the development of characteristic odours in the pubic region. Corynebacterium species produce enzymes that break down proteins and lipids in sweat, generating various compounds that can crystallise and adhere to hair shafts. This process is particularly active in individuals with hyperhidrosis or those who engage in activities that promote excessive sweating. The resulting white deposits often have a distinctly chalky appearance and may be accompanied by discolouration of undergarments or swimwear.
Risk factors for bacterial biofilm formation include poor hygiene practices, excessive sweating, tight-fitting synthetic clothing, and the use of occlusive personal care products. Individuals living in hot, humid climates or those with occupations involving physical labour may be particularly susceptible to these conditions. Treatment typically involves thorough cleansing with antibacterial soaps, the application of topical antibiotics such as clindamycin or erythromycin, and modifications to hygiene routines to prevent recurrence. In some cases, complete hair removal from the affected area may be necessary to eliminate established bacterial biofilms effectively.
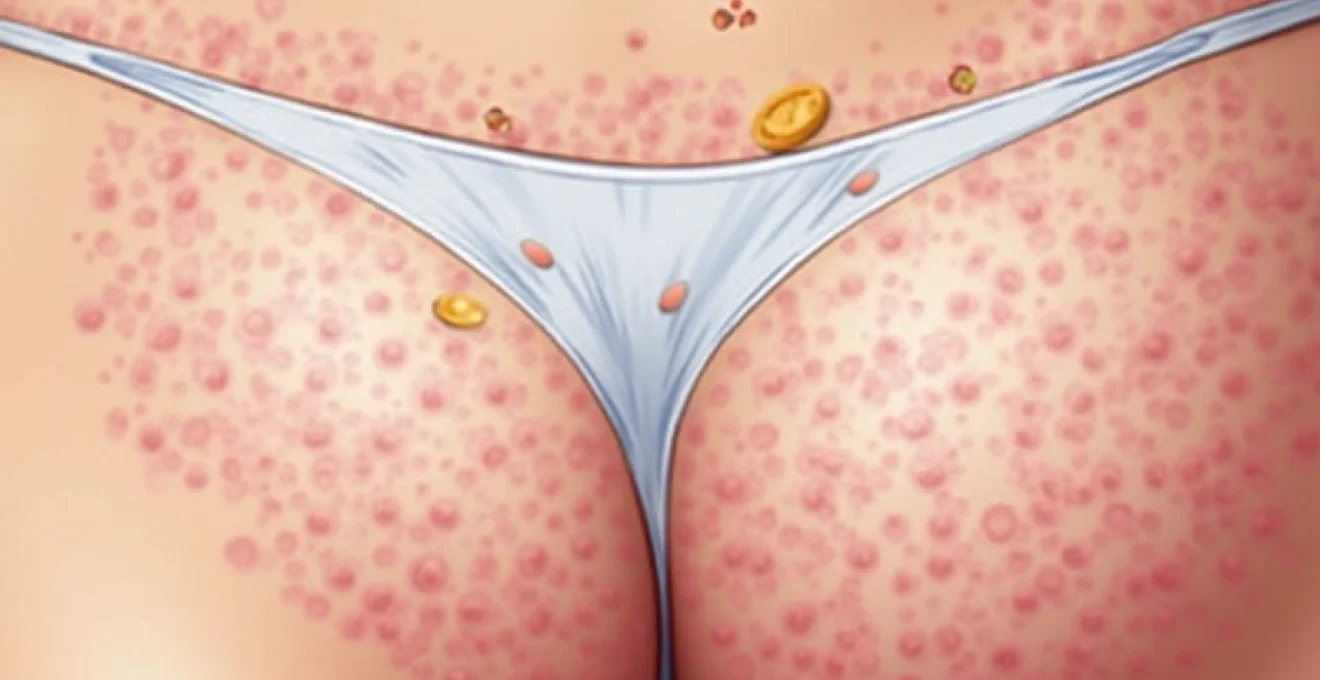
Parasitic infestations and associated white deposits
Parasitic infestations of the pubic region can produce various white substances that may be mistaken for natural deposits or other benign conditions. These parasites, ranging from microscopic mites to visible insects, create distinctive white materials through their life cycles, feeding activities, and waste production. Understanding the characteristics of parasite-associated white deposits is crucial for accurate diagnosis and appropriate treatment, as these conditions often require specific therapeutic approaches and may indicate the need for partner treatment or environmental decontamination measures.
Phthirus pubis nit attachment mechanisms
Pubic lice, scientifically known as Phthirus pubis, attach their eggs (nits) to pubic hair shafts using a powerful adhesive substance that appears white or cream-coloured. These nits are oval-shaped, approximately 1mm in length, and firmly cemented to the base of hair shafts near the skin surface. The white appearance of nits can be particularly noticeable on darker hair, creating the illusion of white coating along multiple hair strands. Unlike other white substances on pubic hair, nits cannot be easily removed by washing or brushing and require specific treatments or manual extraction with fine-toothed combs. The presence of nits often accompanies adult lice, which appear as small, greyish-white insects that may be visible to the naked eye during careful examination.
Demodex folliculorum mite activity in hair follicles
Demodex folliculorum mites, microscopic arthropods that naturally inhabit hair follicles, can sometimes proliferate excessively in the pubic region, leading to the production of white, waxy substances around hair shafts. These mites feed on dead skin cells and sebaceous secretions, producing waste products that can accumulate as white or cream-coloured deposits. Demodex overgrowth often occurs in individuals with compromised immune systems, elderly patients, or those using immunosuppressive medications. The resulting white deposits may be accompanied by follicular inflammation, redness, and itching. Diagnosis requires microscopic examination of affected hair follicles, and treatment typically involves topical acaricides or oral medications in severe cases.
Sarcoptes scabiei burrow debris and skin flakes
Scabies mites, while primarily affecting skin rather than hair directly, can create white, flaky debris in the pubic region through their burrowing activities. These microscopic parasites create tunnels in the upper layers of skin, producing waste products and causing inflammatory responses that result in white scaling and flaking around pubic hair. The debris consists of mite feces, eggs, and sloughed skin cells that can accumulate on hair shafts and in the surrounding area. Scabies infestations are characteristically intensely itchy, particularly at night, and may be accompanied by small, red bumps or burrow tracks. The condition is highly contagious and requires prompt treatment with prescription scabicides to prevent spread to close contacts.
Dermatological conditions producing white flaking
Several dermatological conditions can manifest in the pubic region, producing white flaking or scaling that may coat pubic hair. These conditions often involve disruptions to normal skin cell turnover, inflammatory processes, or autoimmune responses that result in excessive production of white, flaky material. Seborrhoeic dermatitis represents one of the most common dermatological causes of white flaking in hair-bearing areas, including the pubic region. This inflammatory condition results from an overgrowth of Malassezia yeasts combined with an inflammatory response that varies among individuals based on genetic predisposition and environmental factors.
Psoriasis occasionally affects the pubic region, producing thick, silvery-white scales that can coat hair shafts and create the appearance of white substance accumulation. Unlike other conditions, psoriatic scaling typically appears as thick, adherent plaques with well-defined borders and may extend beyond the hair-bearing areas. The scales in genital psoriasis are often softer and less silvery than those found in other body regions due to the warm, moist environment, but they still create distinctive white deposits on pubic hair.
Contact dermatitis resulting from allergic reactions to personal care products, detergents, or synthetic fabrics can produce white, flaky skin that adheres to pubic hair. This condition often develops gradually as sensitivity builds to specific ingredients such as fragrances, preservatives, or chemical irritants. The inflammatory response leads to increased skin cell turnover and the production of white, scaly material that can coat hair shafts. Identifying and avoiding the triggering substances is essential for resolution, along with appropriate anti-inflammatory treatments.
Lichen sclerosus , an autoimmune condition affecting genital skin, can produce white, papery skin changes and scaling that may extend to involve pubic hair. This condition primarily affects the vulvar and anal regions but can occasionally involve hair-bearing areas, creating white, atrophic patches with associated scaling. The white material produced by lichen sclerosus has a characteristic tissue-paper appearance and may be accompanied by intense itching, pain, or burning sensations. Early diagnosis and treatment with topical corticosteroids are crucial to prevent permanent scarring and functional impairment.
Topical product residue and chemical interactions
Modern personal care routines often involve the application of various topical products to the pubic region, including soaps, shampoos, conditioners, moisturisers, depilatories, and specialised intimate hygiene products. Many of these formulations contain ingredients that can leave white residues on pubic hair, particularly when products are not thoroughly rinsed away or when multiple products are used in combination. Understanding how these residues form and accumulate helps distinguish between product-related white deposits and those indicating underlying medical conditions.
Antiperspirants and deodorants applied to the pubic region often contain aluminium compounds, talc, and other white powders that can create visible deposits on hair shafts. These products are designed to reduce sweating and control odour, but their active ingredients can crystallise and adhere to hair, particularly in areas where moisture and friction are common. The resulting white deposits may appear chalky or powdery and can be accompanied by product build-up that resists removal with ordinary washing. Some individuals may develop sensitivity reactions to these products, leading to additional white flaking from inflammatory skin responses.
Intimate washes and feminine hygiene products frequently contain surfactants, emulsifiers, and conditioning agents that can leave white, waxy residues on pubic hair. These products are often formulated to be gentle on sensitive genital tissues, but their moisturising and conditioning components can accumulate over time, particularly in individuals with coarse or chemically-treated hair. The residues may appear as white, creamy deposits that feel smooth or slightly sticky to the touch and may trap environmental particles and dead skin cells.
Hair removal products, including depilatory creams and pre-shave preparations, can
leave white, chalky residues on pubic hair that persist even after the product has served its intended purpose. These chemical formulations often contain calcium thioglycolate, potassium thioglycolate, or other alkaline compounds that break down hair proteins. When these products interact with natural oils and moisture in the pubic region, they can form white precipitates that coat remaining hair shafts. The residues may have a slightly gritty texture and can be particularly noticeable in individuals who use these products frequently or fail to rinse thoroughly after application.
Soap scum and hard water deposits represent another significant source of white substance accumulation on pubic hair. When soaps containing fatty acids or glycerin are used in areas with hard water, the interaction between soap molecules and mineral ions creates insoluble precipitates that appear as white, filmy deposits. These deposits can be particularly stubborn and may require specific removal techniques using acidic solutions or chelating agents. The problem is often exacerbated by the use of bar soaps or products containing high concentrations of calcium or magnesium stearate.
Chemical interactions between different personal care products can create unexpected white deposits through precipitation reactions or emulsion breakdown. For example, the combination of acidic intimate washes with alkaline deodorants can produce white, curdled precipitates that adhere strongly to hair shafts. Similarly, the layering of oil-based moisturisers with water-based cleansers can result in emulsion instability and the formation of white, separated phases that coat pubic hair. Understanding product chemistry and avoiding incompatible combinations can help prevent these unwanted interactions.
Fabric softeners and laundry detergents used on undergarments can transfer to pubic hair through direct contact, creating white, waxy residues that accumulate over time. These products contain cationic surfactants and conditioning agents designed to soften fabrics, but they can also deposit on skin and hair surfaces. The residues may appear as white, slightly sticky coatings that trap lint and other particles, creating a more pronounced white appearance. Individuals sensitive to these chemicals may also develop inflammatory responses that contribute to additional white flaking and scaling.
Prevention of product-related white deposits involves careful selection of compatible formulations, thorough rinsing after product application, and periodic deep cleansing to remove accumulated residues. Using pH-balanced products specifically designed for intimate areas can help minimise the risk of chemical interactions and precipitation. When multiple products must be used, allowing adequate time between applications and ensuring complete removal of previous products can prevent unwanted chemical reactions. Regular exfoliation with gentle mechanical methods can help remove stubborn product build-up while maintaining the health of underlying skin and hair follicles.