The mandibular incisors, commonly known as the bottom front teeth, represent one of the most vulnerable tooth structures in the oral cavity when it comes to pathological wear patterns. Unlike the posterior teeth that primarily handle grinding forces during mastication, these delicate anterior teeth face unique challenges that make them particularly susceptible to premature deterioration. Understanding the complex interplay of anatomical, functional, and pathological factors that contribute to lower incisor wear is essential for both dental professionals and patients seeking to preserve their oral health.
The phenomenon of bottom front tooth wear affects millions of individuals worldwide, often progressing silently until significant structural damage has occurred. This wear pattern can result from various mechanisms including mechanical attrition, chemical erosion, and abrasive forces that gradually compromise the protective enamel layer. The consequences extend far beyond aesthetic concerns , potentially leading to increased tooth sensitivity, structural weakness, and the need for extensive restorative treatment.
Anatomical structure and occlusal forces affecting mandibular incisors
The mandibular incisors possess unique anatomical characteristics that predispose them to wear patterns distinct from other tooth types. These teeth serve as the primary cutting instruments during mastication, positioning them at the forefront of functional forces within the oral cavity. The structural design of lower front teeth reflects their specialised role, featuring thin incisal edges optimised for shearing food particles rather than withstanding heavy compressive forces.
Enamel thickness variations in lower anterior teeth
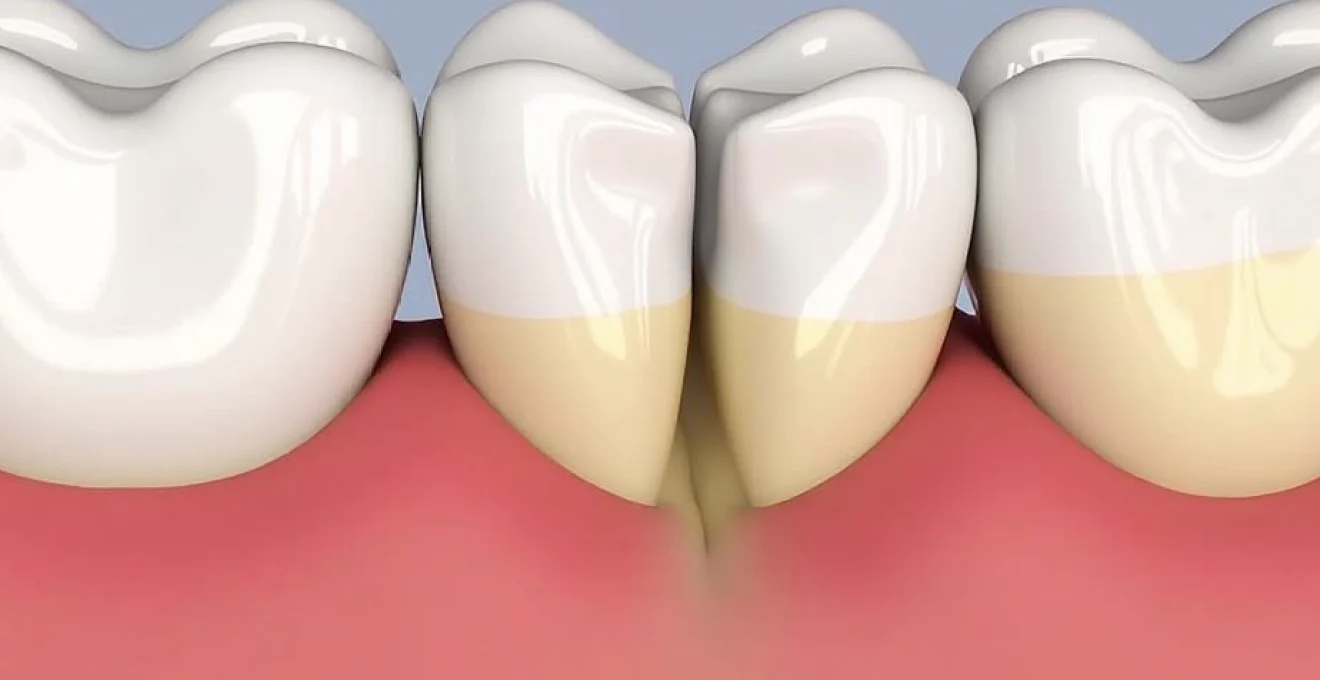
The enamel thickness distribution across mandibular incisors creates inherent vulnerabilities that contribute to accelerated wear patterns. Research indicates that the incisal edges of lower front teeth possess enamel layers measuring approximately 1.0-1.5 millimetres in thickness, significantly thinner than the 2.5-3.0 millimetres found on molar cusps. This reduced protective coating means that even moderate increases in functional stress can rapidly compromise the underlying dentin structure.
The cervical regions of these teeth present additional challenges, with enamel thickness diminishing to less than 0.5 millimetres near the cemento-enamel junction. This anatomical variation explains why many patients experience sensitivity and wear patterns that begin at the gumline and progress towards the incisal edges. The progressive nature of this wear pattern often catches patients unaware until significant structural loss has occurred.
Masticatory force distribution patterns on central and lateral incisors
During normal function, mandibular incisors experience force distributions that differ markedly from posterior teeth. Bite force measurements reveal that these teeth typically encounter forces ranging from 150-300 Newtons during normal function, but this can increase dramatically under pathological conditions. The central incisors bear approximately 60% of anterior loading forces, whilst the lateral incisors handle the remaining 40%.
The angle of force application plays a crucial role in wear progression. When forces are applied perpendicular to the incisal edge, the tooth structure can effectively distribute stress throughout the root and supporting tissues. However, lateral or oblique forces create shear stresses that concentrate along specific contact points, leading to localised wear patterns and potential structural failure.
Root morphology impact on stress concentration points
The single-rooted configuration of mandibular incisors creates unique stress distribution characteristics that influence wear patterns. Unlike multi-rooted teeth that can distribute forces across multiple root surfaces, the narrow, ribbon-like roots of lower front teeth concentrate stresses within a limited cross-sectional area. This concentration effect amplifies the impact of excessive forces on the crown structure.
The root-to-crown ratio in mandibular incisors typically measures 1:1 to 1.2:1, providing adequate support under normal conditions. However, when subjected to excessive lateral forces or increased functional demands, this ratio becomes insufficient to prevent harmful stress concentrations at the cervical region. This mechanical disadvantage contributes to the characteristic wedge-shaped defects often observed in these teeth.
Periodontal ligament response to excessive loading forces
The periodontal ligament surrounding mandibular incisors exhibits specific responses to mechanical overloading that can exacerbate wear patterns. Under normal conditions, this specialised connective tissue provides shock absorption and proprioceptive feedback. However, chronic excessive forces can lead to adaptive changes that compromise its protective function.
Studies demonstrate that sustained overloading triggers inflammatory responses within the periodontal space, leading to localised bone remodelling and potential tooth mobility. This mobility creates micro-movements during function that can accelerate wear at contact points. The resulting feedback loop of increased mobility and progressive wear often requires interceptive treatment to prevent further deterioration.
Bruxism and Parafunction-Related attrition mechanisms
Bruxism represents the most significant pathological contributor to mandibular incisor wear, affecting an estimated 8-31% of the adult population. This parafunctional habit involves the grinding, clenching, or gnashing of teeth outside of normal functional activities, creating forces that can exceed normal chewing loads by factors of 10-20. The repetitive nature of these movements, combined with the sustained duration typical of nocturnal episodes, creates ideal conditions for accelerated tooth wear.
The relationship between bruxism and anterior tooth wear involves complex neurological, psychological, and mechanical factors. Sleep-related bruxism episodes can generate forces exceeding 1,000 Newtons, applied rhythmically over periods lasting several hours. This sustained loading overwhelms the natural protective mechanisms that typically prevent excessive tooth wear during normal function.
Nocturnal grinding patterns and mandibular incisor contact points
Polysomnographic studies reveal that nocturnal bruxism episodes follow predictable patterns that particularly affect mandibular incisors. During typical grinding sequences, the mandible moves through lateral excursions that bring the incisal edges of lower teeth into heavy contact with the lingual surfaces of maxillary incisors. This contact pattern creates concentrated wear facets along the incisal edges and lingual aspects of the lower front teeth.
The duration and intensity of nocturnal grinding episodes vary significantly among individuals, with some patients exhibiting brief, high-intensity bursts whilst others demonstrate prolonged, moderate-intensity grinding patterns. Research indicates that the cumulative wear effect correlates more closely with episode duration than with peak force measurements, explaining why some patients develop severe wear despite reporting minimal awareness of their grinding habit.
Clenching forces and compressive stress on lower front teeth
Clenching behaviours create compressive stresses that affect mandibular incisors differently than grinding movements. During sustained clenching episodes, the teeth are held in static contact under high force levels, creating isometric loading conditions. This type of loading concentrates stress within the tooth structure itself rather than creating the sliding wear patterns associated with grinding movements.
The compressive nature of clenching forces can lead to internal structural changes within the tooth, including microscopic crack formation and stress concentration at the dentino-enamel junction. These internal changes may not be immediately visible but can predispose teeth to sudden fractures or accelerated wear once the protective enamel layer becomes compromised.
Sleep bruxism EMG activity and tooth wear correlation
Electromyographic studies of masticatory muscles during sleep bruxism episodes reveal specific activation patterns that help explain the preferential wear of mandibular incisors. The masseter and temporalis muscles show coordinated activation during grinding episodes, with the lateral pterygoid muscles providing the guidance for mandibular excursions that bring the anterior teeth into contact.
Quantitative EMG analysis demonstrates that bruxism episodes involving anterior guidance patterns generate higher wear rates on mandibular incisors compared to episodes limited to posterior tooth contact. The anterior guidance mechanism, whilst protective during normal function, becomes destructive when activated under the excessive forces typical of bruxism events.
Awake bruxism triggers and daytime parafunction habits
Daytime bruxism presents unique challenges for mandibular incisor preservation, often manifesting as unconscious clenching or grinding triggered by stress, concentration, or specific environmental factors. Unlike sleep bruxism, awake parafunction can potentially be controlled through conscious awareness and behavioural modification techniques.
Common triggers for daytime bruxism include work-related stress, driving, computer use, and physical exertion. The forces generated during awake bruxism typically measure lower than nocturnal episodes but occur with greater frequency throughout the day. This constant low-level loading can create fatigue failure in tooth structures, leading to progressive wear that may not correlate with the perceived intensity of the habit.
Malocclusion classifications contributing to anterior tooth wear
Malocclusion creates mechanical imbalances that significantly contribute to pathological wear patterns in mandibular incisors. When teeth are not properly aligned, normal functional forces are redirected in ways that concentrate stress on specific tooth surfaces, leading to accelerated wear. The classification of malocclusion provides insight into the mechanical factors that predispose certain individuals to anterior tooth wear problems.
Understanding the relationship between specific occlusal relationships and wear patterns enables targeted preventive interventions. Early identification of malocclusion-related wear risks allows for interceptive orthodontic treatment or occlusal adjustments that can prevent or minimise future tooth structure loss.
Class II division 2 deep overbite and incisal edge trauma
Class II Division 2 malocclusion creates particularly destructive conditions for mandibular incisors through excessive overbite relationships. In this configuration, the maxillary incisors are retroclined and create deep vertical overlap with the mandibular incisors, often exceeding 4-5 millimetres of overbite. This relationship positions the lower front teeth to contact the lingual surfaces of upper teeth during function, creating traumatic contact that accelerates wear.
The deep overbite mechanism concentrates forces on the incisal third of mandibular incisors, creating characteristic wear patterns that progress from the cutting edges towards the cervical regions. Patients with untreated deep overbite relationships often develop significant wear by their third decade of life, requiring extensive restorative treatment to restore proper function and aesthetics.
Anterior crossbite mechanics and abnormal wear patterns
Anterior crossbite conditions reverse the normal occlusal relationship, positioning one or more mandibular incisors labial to their maxillary counterparts. This reversal creates abnormal contact patterns during function, often resulting in edge-to-edge contact or interference during mandibular excursions. The mechanical disadvantage created by this relationship accelerates wear on both the affected mandibular incisors and their maxillary opponents.
The wear pattern in anterior crossbite situations typically involves the labial surfaces of mandibular incisors, contrasting with the more common lingual and incisal wear seen in normal occlusal relationships. This unique wear distribution can create aesthetic concerns earlier in the progression, often motivating patients to seek treatment before severe structural damage occurs.
Edge-to-edge bite relationship and attrition acceleration
Edge-to-edge anterior relationships eliminate the normal protective overbite and overjet that typically prevent excessive contact between opposing incisors. In this configuration, the incisal edges of mandibular and maxillary incisors meet directly during closure and function, creating ideal conditions for rapid attrition of both tooth groups.
The accelerated wear associated with edge-to-edge relationships often progresses symmetrically, affecting multiple teeth simultaneously. This pattern can lead to loss of vertical dimension and subsequent over-closure, creating additional mechanical problems throughout the masticatory system. Early intervention in edge-to-edge relationships can prevent the cascade of problems associated with progressive anterior wear.
Crowding-induced contact point alterations
Dental crowding in the anterior region creates localised areas of increased contact pressure that contribute to accelerated wear patterns. When mandibular incisors are crowded, normal contact relationships are disrupted, leading to point contacts rather than the broad area contacts that characterise ideal occlusion. These point contacts concentrate forces over smaller surface areas, increasing the stress per unit area and accelerating local wear.
The irregular contact patterns associated with crowding also create areas of food impaction and plaque retention that can contribute to erosive wear processes. The combination of mechanical and chemical factors in crowded anterior regions often creates complex wear patterns that require comprehensive treatment approaches addressing both the mechanical and biological aspects of the problem.
Gastroesophageal reflux disease and dental erosion pathways
Gastroesophageal reflux disease (GERD) presents a significant chemical threat to mandibular incisors through the chronic exposure to gastric acids. The lingual surfaces of lower front teeth are particularly vulnerable to acid erosion due to their proximity to the source of refluxed gastric contents and the pooling effect that occurs when patients are in supine positions during sleep. The pH of gastric acid typically measures between 1.5-2.0, well below the critical pH of 5.5 required for enamel demineralisation.
The erosive process differs markedly from mechanical wear, creating smooth, polished surfaces rather than the roughened appearance typical of attrition. GERD-related erosion often begins on the lingual surfaces of mandibular incisors, gradually progressing to involve the entire crown structure as the condition persists. The silent nature of this erosive process means that significant tooth structure can be lost before patients become aware of the problem through increased sensitivity or aesthetic changes.
Studies indicate that individuals with GERD demonstrate enamel loss rates 3-5 times higher than healthy controls, with the mandibular incisors showing the most pronounced changes. The chronic nature of reflux episodes, particularly nocturnal reflux, creates sustained acid exposure that overwhelms the natural buffering capacity of saliva. This prolonged demineralisation process weakens the tooth structure, making it more susceptible to mechanical wear from normal functional forces.
The relationship between GERD and tooth wear extends beyond direct chemical erosion to include secondary effects on oral physiology. Patients with GERD often experience reduced salivary flow and altered saliva composition, compromising the natural protective mechanisms that normally prevent acid-related tooth damage. Additionally, medications commonly prescribed for GERD management can further reduce salivary function, creating a compound effect that accelerates tooth wear progression.
Age-related physiological changes in tooth structure
The natural ageing process brings about significant changes in tooth structure that predispose mandibular incisors to increased wear rates. As individuals age, the enamel layer undergoes structural modifications that reduce its resistance to both mechanical and chemical challenges. The crystalline structure of aged enamel becomes more porous and less organised, creating pathways for acid penetration and reducing the overall strength of the protective layer.
Dentin sclerosis represents another age-related change that affects wear patterns in mandibular incisors. As secondary dentin formation continues throughout life, the pulp chamber gradually reduces in size whilst the dentin becomes more mineralised and brittle. This increased brittleness makes aged teeth more susceptible to fracture under normal functional loads, often manifesting as chipping or sudden structural failure at the incisal edges.
Salivary changes associated with ageing significantly impact the oral environment’s ability to protect against tooth wear. Reduced salivary flow rates and altered saliva composition decrease the mouth’s natural buffering capacity and remineralisation potential. The decreased salivary lubrication also increases friction during functional movements, contributing to accelerated mechanical wear of tooth surfaces.
The cumulative effect of decades of functional loading creates fatigue failure patterns in aged mandibular incisors. Microscopic cracks that develop over years of service gradually propagate through the tooth structure, eventually leading to visible wear patterns or sudden structural failure. This fatigue phenomenon explains why many patients experience accelerated tooth wear in their sixth and seventh decades of life, even in the absence of obvious pathological factors.
Research demonstrates that individuals over 65 years of age show mandibular incisor wear rates approximately 2.5 times higher than those in their third decade of life, even when controlling for pathological factors such as bruxism or GERD.
Preventive strategies and occlusal therapy interventions
Effective prevention of mandibular incisor wear requires a comprehensive approach that addresses the multiple contributing factors identified in contemporary research. The most successful preventive strategies combine patient education, behavioural modification techniques, and targeted therapeutic interventions tailored to individual risk profiles. Understanding that tooth wear represents a multifactorial process enables clinicians to develop personalised prevention protocols that address the specific combination of factors affecting each patient.
Occlusal
analysis reveals that targeted occlusal adjustments can reduce excessive loading on mandibular incisors by redistributing forces across the entire dental arch. Selective reshaping of opposing tooth surfaces eliminates premature contacts that concentrate stress on vulnerable anterior teeth, whilst equilibration procedures establish balanced bilateral contact patterns during functional movements.
Night guard therapy represents one of the most effective interventions for patients exhibiting bruxism-related wear patterns. Custom-fabricated occlusal splints provide a protective barrier between opposing teeth whilst redistributing forces across broader contact areas. Research indicates that properly designed night guards can reduce mandibular incisor wear rates by up to 85% in patients with documented nocturnal bruxism habits.
The success of splint therapy depends heavily on proper design considerations that address individual patient needs. Hard acrylic resin splints provide superior durability for heavy bruxers, whilst softer materials may be indicated for patients with temporomandibular joint sensitivities. The occlusal surface design must incorporate appropriate guidance patterns that protect anterior teeth during lateral excursions whilst maintaining stable posterior support.
Pharmaceutical interventions targeting underlying bruxism mechanisms show promise in reducing parafunctional activity. Muscle relaxants, anti-anxiety medications, and botulinum toxin injections can reduce the intensity and frequency of grinding episodes, providing additional protection for vulnerable mandibular incisors. However, these approaches require careful consideration of potential side effects and should be integrated with other preventive measures for optimal results.
Dietary counselling plays a crucial role in preventing erosive tooth wear, particularly in patients with identified acid exposure risks. Limiting acidic beverages, timing acid consumption to minimise tooth contact, and implementing post-exposure rinsing protocols can significantly reduce chemical erosion rates. Patients should be educated about the delayed brushing protocol, waiting at least 30-60 minutes after acid exposure before performing oral hygiene procedures to prevent abrading softened enamel surfaces.
Early orthodontic intervention can address malocclusion-related wear risks before significant tooth structure loss occurs. Correcting deep overbite relationships, resolving anterior crossbites, and eliminating crowding-induced contact point problems can prevent the development of pathological wear patterns. The timing of orthodontic treatment becomes critical, as intervention during adolescence or early adulthood provides the greatest protective benefit for long-term tooth preservation.
Clinical studies demonstrate that patients who receive comprehensive preventive care combining occlusal therapy, behavioural modification, and regular monitoring show 70% less mandibular incisor wear progression over five-year periods compared to those receiving routine dental care alone.
Regular monitoring protocols enable early detection of wear progression before significant structural damage occurs. Digital photography, study models, and quantitative wear measurement techniques provide objective documentation of changes over time. This data-driven approach allows for timely intervention adjustments and helps predict future treatment needs, enabling proactive rather than reactive management strategies.
Patient education represents the cornerstone of successful long-term wear prevention. Individuals must understand the multifactorial nature of tooth wear and their role in implementing protective behaviours. This includes recognising early warning signs of excessive wear, understanding the relationship between lifestyle factors and oral health, and maintaining compliance with recommended preventive measures.
The integration of modern technology into preventive protocols offers new opportunities for enhanced patient care. Smartphone applications can help patients track bruxism episodes, monitor dietary acid exposure, and maintain compliance with preventive recommendations. Wearable devices that detect grinding activity provide real-time feedback that can help modify harmful behaviours before significant tooth damage occurs.
Success in preventing mandibular incisor wear ultimately depends on addressing the specific combination of risk factors present in each individual case. A 45-year-old patient with GERD and moderate bruxism requires a different preventive approach than a 25-year-old with severe crowding and high dietary acid intake. This personalised medicine approach ensures that preventive resources are allocated efficiently whilst maximising protective benefits for vulnerable tooth structures.